
Human Corneal Epithelial Cells
Cat.No.: CSC-C9224J
Species: Human
Source: Cornea; Eye
Cell Type: Epithelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Human corneal epithelial cells come from the cornea which produces a transparent tissue that covers one-sixth of the eye's anterior surface and displays unique structural and functional properties. The cornea is composed of five layers, from the outside to the inside: the epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium. As the outermost corneal layer, the corneal epithelium comprises one layer of non-keratinized stratified squamous epithelial cells. Tight junctions firmly link these cells together to create an efficient barrier against water loss and pathogen entry. When corneal damage occurs corneal epithelial cells swiftly migrate to the damaged area to restore tissue integrity through movement, division, and differentiation processes.
Due to its transparent nature and lack of blood vessels the cornea serves as an ideal model for drug permeability and toxicity research. Scientists produce transplantation-ready corneal tissues by cultivating corneal epithelial cells in laboratory conditions. The developed tissues provide treatment solutions for corneal diseases and injuries. The models also allow researchers to explore disease development processes in corneal conditions including corneal fibrosis and diabetic keratopathy.
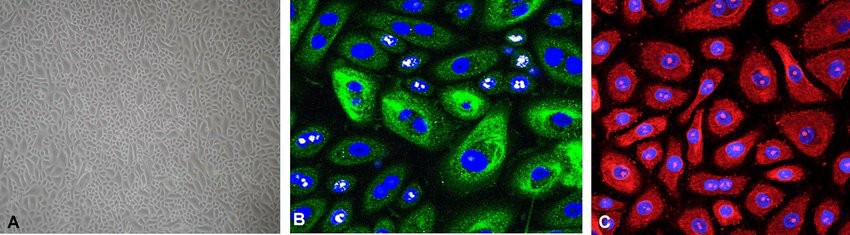 Fig. 1. Characterization of normal human corneal epithelial cells during expansion in a monolayer culture (Kaluzhny Y, Kinuthia M, et al., 2018).
Fig. 1. Characterization of normal human corneal epithelial cells during expansion in a monolayer culture (Kaluzhny Y, Kinuthia M, et al., 2018).
Ni exposure Decreased Cell Viability and Altered Cell Morphology of Human Corneal Epithelial Cells
External pollutants such as heavy metals damage human corneal epithelial cells (HCEC) by disrupting their function. Zhang's team examined the toxic effects of nickel (Ni) on HCEC by measuring cell viability and morphology since these factors indicate cytotoxic effects. They employed HCEC cells extracted from healthy human eyes to achieve dependable outcomes. A preliminary experiment determined the lethal concentration (LC50) of Ni to be 248.8 μM, leading to the selection of 1 μM, 10 μM, and 100 μM for further testing (Fig. 1B). These concentrations are within environmentally relevant and in vivo ranges. Results showed no significant viability difference between the control and 1 μM Ni group (Fig. 1E), with normal cell morphology. However, 10 μM Ni slightly decreased viability by 5% (Fig. 1C and F), and 100 μM Ni significantly reduced viability to 76%, with many cells showing abnormal shapes and floating (Fig. 1C and G). This indicates that Ni cytotoxicity increases with concentration, potentially through oxidative stress or DNA repair inhibition.
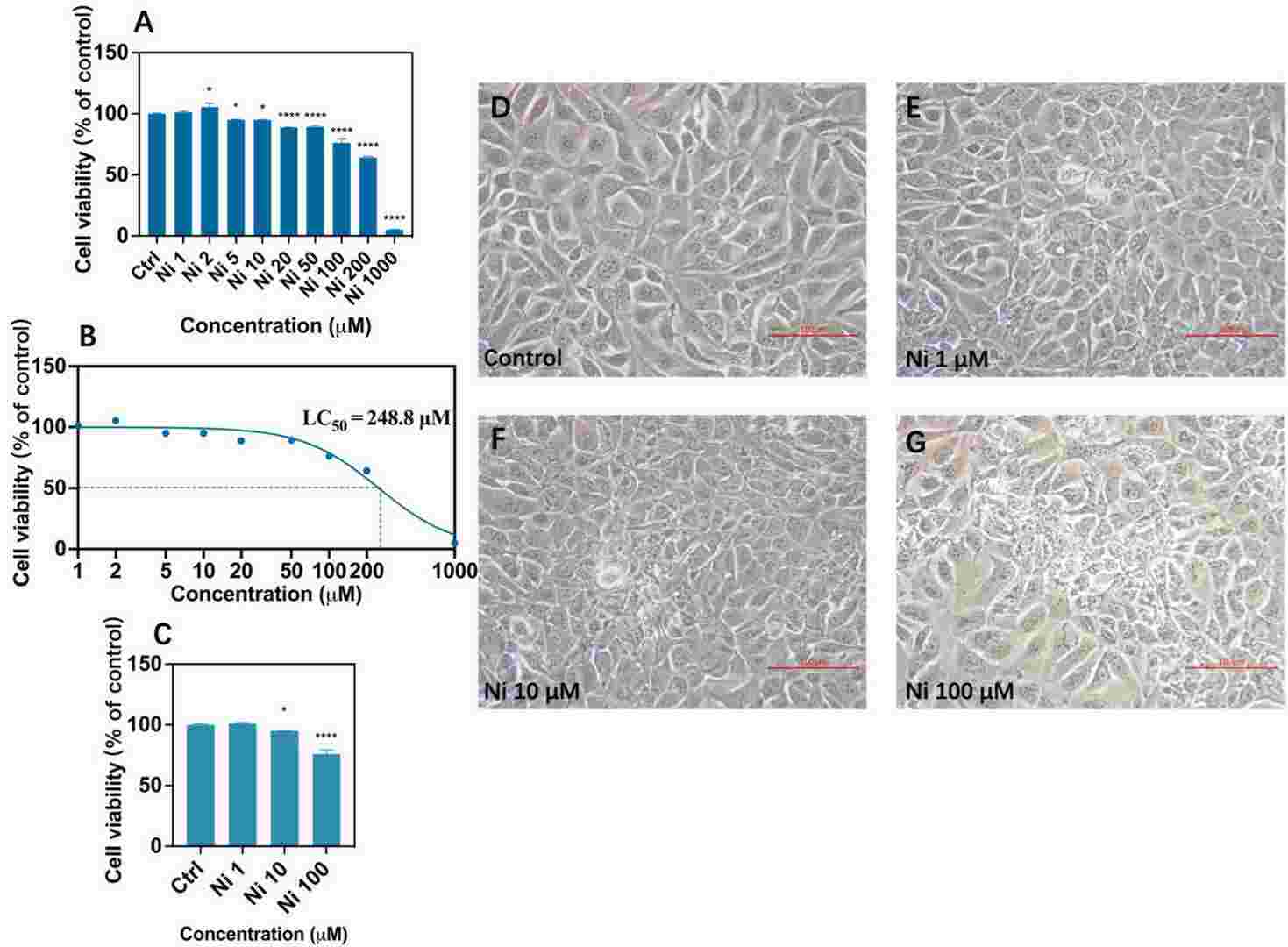 Fig. 1. Cell viability after Ni exposure (A, C) and LC50 calculated by nonlinear fitting after logarithmic conversion of concentration after Ni exposure (B) and morphological changes of human corneal epithelial cells by inverted microscope (TS-100, Nikon, Tokyo, Japan) at 200× magnification (D-G) after exposure to Ni for 24 h (Zhang ZN, Liu H, et al., 2022).
Fig. 1. Cell viability after Ni exposure (A, C) and LC50 calculated by nonlinear fitting after logarithmic conversion of concentration after Ni exposure (B) and morphological changes of human corneal epithelial cells by inverted microscope (TS-100, Nikon, Tokyo, Japan) at 200× magnification (D-G) after exposure to Ni for 24 h (Zhang ZN, Liu H, et al., 2022).
Esculetin Protected HCE Cells Against Cytotoxicity Induced by H2O2 Treatment
Oxidative stress triggers multiple ocular conditions including dry eye that presents symptoms of discomfort along with tear film instability. The condition arises when reactive oxygen species outnumber antioxidants in the body. Esculetin, found in plants and traditional Chinese medicine "Qinpi," has antioxidant properties, but its mechanisms in protecting corneal epithelial cells are unknown. Zhang's team explored the protective impact of esculetin on human corneal epithelial (HCE) cells by conducting experiments in both in vitro and in vivo models.
The researchers demonstrated that cell proliferation increased slightly when cells were exposed to 0.01-100 μM esculetin for 24 hours without causing cytotoxic effects (Fig. 2A). They implemented an oxidative stress model induced by H2O2. Cell viability displayed a dose-dependent decline after 24 hours of H2O2 treatment with 800 μM H2O2 reducing survival to 46% (Fig. 2B). All following experiments utilized an H?O? concentration of 800 μM. A pretreatment of cells with 10-100 μM esculetin for 2 hours before 24 hours of 800 μM H2O2 exposure raised cell viability levels according to dose dependency (Fig. 2C). Cell viability improved from 30.42% ± 0.29% to 81.56% ± 1.99% when pre-treated with esculetin.
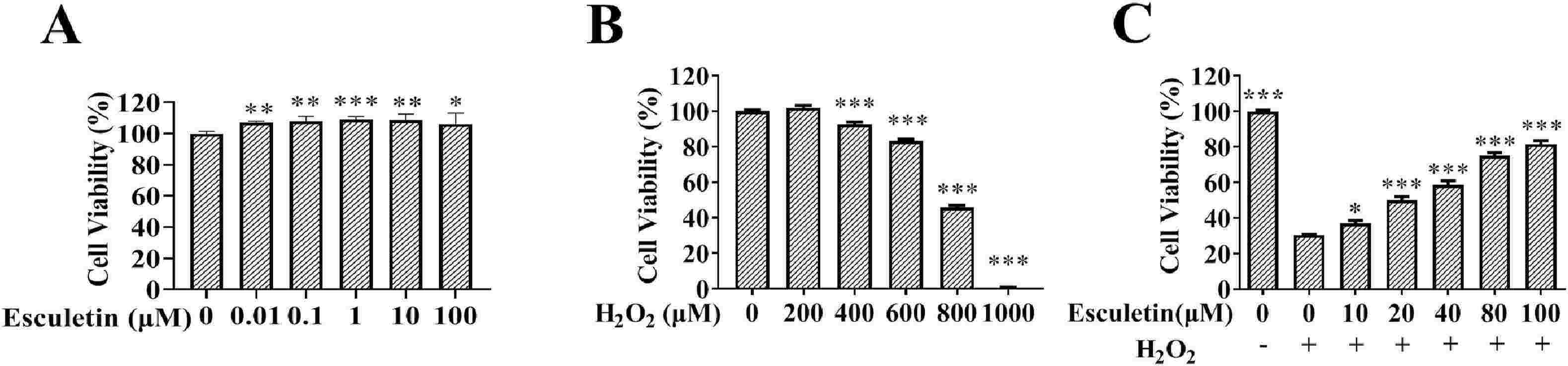 Fig. 2. Pretreatment with esculetin increased the cell viabilities in H2O2-treated HCE cells (Zhang YJ, An YL, et al., 2021).
Fig. 2. Pretreatment with esculetin increased the cell viabilities in H2O2-treated HCE cells (Zhang YJ, An YL, et al., 2021).
Creative Bioarray can provide primary and immortalized Human Corneal Epithelial Cells for you.
Ask a Question
Write your own review



