Isoproterenol-induced Heart Failure Model
Isoproterenol, a nonselective beta-adrenergic agonist, cause cardiac injury and is commonly used in the study of heart disease. These models are classified into acute and chronic heart failure depending on the dose and duration of isoproterenol administration. Isoproterenol induced acute heart failure is a model characterized by acute apical segment ventricular dysfunction, simulating stress-induced cardiomyopathy (SIC) in human. Besides, the chronic model mimics advanced heart failure in humans. These models provides tools to study structural and functional adaptation of myocardium during the progression of heart failure.
Creative Bioarray specializes in providing customized pharmacodynamic research services to help customers assess the efficacy of drug candidates and study the associated pathological mechanisms through isoproterenol-induced heart failure model.
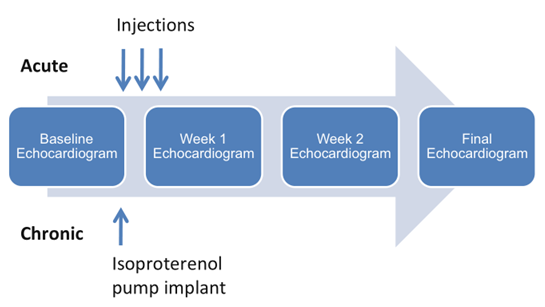 Figure. 1. Acute and chronic isoproterenol models
Figure. 1. Acute and chronic isoproterenol models
Species available
- Mouse
- Rat
Our Capabilities
- We detect changes in myocardial morphology by H&E staining and so on.
- We evaluate left ventricular internal diameters in diastole (LVIDD, mm), left ventricular internal diameters in systole (LVIDS, mm) and left ventricular ejection fraction (EF, %) and left ventricular fractional shortening by Echocardiography.
Assays available
- Echocardiography
- Transmission Electron Microscope (TEM)
- Histopathological evaluation
- Biochemical analysis
With extensive experience in the field of cardiovascular diseases, we are confident to help you overcome any upcoming challenges. Our experts are fully capable of customizing our protocols and assays to meet your specific needs. With our help, we wish to facilitate your research with high efficiency.
Study examples
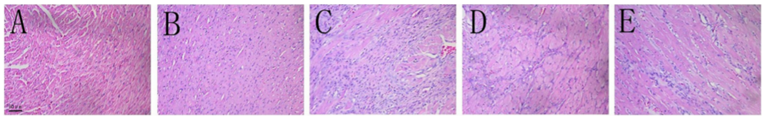 Figure. 2. Effect of OMT on cardiac histopathological changes of ISO-induced heart failure rats (H&E staining 200×). (A) Control. (B) OMT 100 mg/kg. (C) Isoproterenol 5 mg/kg. (D) OMT 100 mg/kg + isoproterenol. (E) OMT 50 mg/kg + isoproterenol.
Figure. 2. Effect of OMT on cardiac histopathological changes of ISO-induced heart failure rats (H&E staining 200×). (A) Control. (B) OMT 100 mg/kg. (C) Isoproterenol 5 mg/kg. (D) OMT 100 mg/kg + isoproterenol. (E) OMT 50 mg/kg + isoproterenol.
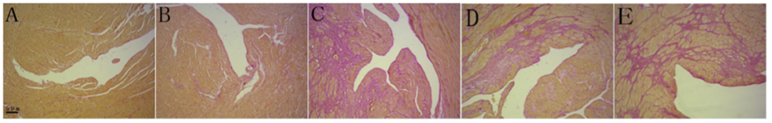 Figure. 3. Representative Van Gieson-stained sections of the cardiac apex (100×). (A) Control. (B) OMT 100 mg/kg. (C) Isoproterenol 5 mg/kg. (D) OMT 100 mg/ kg + isoproterenol. (E) OMT 50 mg/kg + isoproterenol. Red indicates fibrotic regions.(For interpretation of the references to colour in this figure legend,the reader is referred to the web version of this article.)
Figure. 3. Representative Van Gieson-stained sections of the cardiac apex (100×). (A) Control. (B) OMT 100 mg/kg. (C) Isoproterenol 5 mg/kg. (D) OMT 100 mg/ kg + isoproterenol. (E) OMT 50 mg/kg + isoproterenol. Red indicates fibrotic regions.(For interpretation of the references to colour in this figure legend,the reader is referred to the web version of this article.)
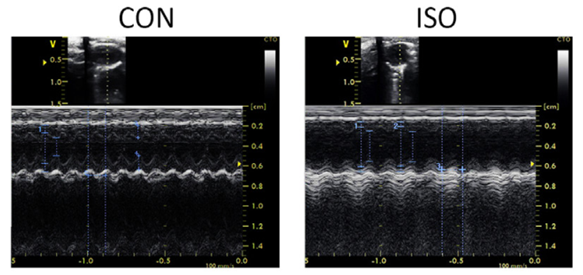 Figure. 4 Representative raw tracings of M-mode echocardiography
Figure. 4 Representative raw tracings of M-mode echocardiography
Quotation and ordering
If you have any special needs or questions regarding our services, please feel free to contact us. We look forward to cooperating with you in the future.
References
Zhou R, et al. Oxymatrine attenuated isoproterenol-induced heart failure in rats via regulation of COX-2/PGI2 pathway[J]. Biomedicine & Pharmacotherapy, 2016:S0753332216311386.
Rui, He, et al. MiR-1a-3p mitigates isoproterenol-induced heart failure by enhancing the expression of mitochondrial ND1 and COX1.[J]. Experimental cell research, 2019.
For research use only. Not for any other purpose.
Disease Models
- Oncology Models
-
Inflammation & Autoimmune Disease Models
- Rheumatoid Arthritis Models
- Glomerulonephritis Models
- Multiple Sclerosis (MS) Models
- Ocular Inflammation Models
- Sjögren's Syndrome Model
- LPS-induced Acute Lung Injury Model
- Peritonitis Models
- Passive Cutaneous Anaphylaxis Model
- Delayed-Type Hypersensitivity (DTH) Models
- Inflammatory Bowel Disease Models
- Systemic Lupus Erythematosus Animal Models
- Oral Mucositis Model
- Asthma Model
- Sepsis Model
- Psoriasis Model
- Atopic Dermatitis (AD) Model
- Scleroderma Model
- Gouty Arthritis Model
- Carrageenan-Induced Air Pouch Synovitis Model
- Carrageenan-Induced Paw Edema Model
- Experimental Autoimmune Myasthenia Gravis (EAMG) Model
- Graft-versus-host Disease (GvHD) Models
-
Cardiovascular Disease Models
- Surgical Models
- Animal Models of Hypertension
- Venous Thrombosis Model
- Atherosclerosis model
- Cardiac Arrhythmia Model
- Hyperlipoidemia Model
- Doxorubicin-induced Heart Failure Model
- Isoproterenol-induced Heart Failure Model
- Arterial Thrombosis Model
- Pulmonary Arterial Hypertension (PAH) Models
- Heart Failure with Preserved Ejection Fraction (HFpEF) Model
- Cardio-Renal-Metabolic (CKM) Syndrome Model
-
Neurological Disease Models
- Alzheimer's Disease Modeling and Assays
- Seizure Models
- Parkinson's Disease Models
- Ischemic Stroke Models
- Acute Spinal Cord Injury (ASCI) Model
- Traumatic Brain Injury (TBI) Model
- Hypoxic-Ischemic Encephalopathy (HIE) Model
- Tourette Syndrome (TS) Model
- Amyotrophic Lateral Sclerosis (ALS) Model
- Huntington's Disease (HD) Model
- Intracerebral hemorrhage (ICH) Models
- Schizophrenia Model
- Depression Models
- Pain Models
-
Metabolic Disease Models
- Type 1 Diabetes Mellitus Model
- Type 2 Diabetes Mellitus Model
- Animal Model of Hyperuricemia
-
Nonalcoholic Fatty Liver Disease Model
- High-Fat Diet-Induced Nonalcoholic Fatty Liver Disease (NAFLD) Model
- Methionine and Choline Deficient (MCD) Diet-Induced Nonalcoholic Fatty Liver Disease (NAFLD) Model
- Gubra-Amylin NASH (GAN) Diet-Induced Nonalcoholic Fatty Liver Disease (NAFLD) Model
- Streptozotocin (STZ) Induced Nonalcoholic Fatty Liver Disease (NAFLD) Model
- High Fat Diet-Induced Obesity Model
- Diabetic Foot Ulcer (DFU) Model
- Cardio-Renal-Metabolic (CKM) Syndrome Model
- Liver Disease Models
- Rare Disease Models
- Respiratory Disease Models
- Digestive Disease Models
-
Urology Disease Models
- Cisplatin-induced Nephrotoxicity Model
- Unilateral Ureteral Obstruction Model
- 5/6 Nephrectomy Model
- Renal Ischemia-Reperfusion Injury (RIRI) Model
- Diabetic Nephropathy (DN) Models
- Passive Heymann Nephritis (PHN) Model
- Adenine-Induced Chronic Kidney Disease (CKD) Model
- Kidney Stone Model
- Doxorubicin-Induced Nephropathy Model
- Orthotopic Kidney Transplantation Model
- Benign Prostatic Hyperplasia (BPH) Model
- Peritoneal Fibrosis Model
- Cardio-Renal-Metabolic (CKM) Syndrome Model
- Orthopedic Disease Models
- Ocular Disease Models
- Skin Disease Models
- Infectious Disease Models
- Otology Disease Models