Colorectal Tumor Cells
- Background
- Applications
- Scientific Data
- FAQ
Colorectal cancer is a significant global health concern, with the incidence and mortality rates steadily rising in recent years. Colorectal tumor cells are abnormal cells that originate in the lining of the colon or rectum, collectively known as the large intestine. These cells exhibit uncontrolled growth, evading the body's natural mechanisms that typically regulate cell division and proliferation. As they continue to multiply, they form a mass or tumor that can eventually spread to other parts of the body, a process known as metastasis.
The heterogeneous nature of colorectal tumor cells is a key factor in the complexity of this disease. These cells can exhibit various genetic and epigenetic alterations, leading to diverse morphological and functional characteristics. This diversity not only challenges the development of effective treatment strategies but also highlights the importance of a comprehensive understanding of the underlying mechanisms driving colorectal cancer progression.
Advantages of In Vitro Cell Line Models for Colorectal Cancer Research
- Experimental control. In vitro cell line models offer precise experimental control, allowing researchers to manipulate and monitor the growth, behavior, and molecular characteristics of colorectal tumor cells under defined conditions. This control is essential for studying specific cellular processes, signaling pathways, and responses to therapeutic agents.
- High reproducibility. Colorectal cancer cell lines provide consistent and reproducible results, enabling researchers to validate experimental findings across multiple studies and laboratories. This reproducibility enhances the reliability of research outcomes and contributes to the robustness of scientific discoveries.
- Cost-effectiveness. In vitro cell line models are generally more cost-effective and logistically feasible compared to in vivo models, enabling a broader range of experiments and high-throughput screening assays. This cost-efficiency allows for the screening of larger compound libraries and the rapid evaluation of potential drug candidates for colorectal cancer treatment.
- Scale and manipulation. Colorectal cancer cell lines can be expanded in large quantities, facilitating experiments requiring substantial cell numbers for molecular analyses, drug testing, and genomic studies. Additionally, these cells can be genetically manipulated to study specific genetic alterations, gene expression profiles, and signaling pathways relevant to colorectal cancer.
Cancer modeling and drug screening
One of the primary applications of colorectal tumor cells is their use in cancer modeling and drug screening. By culturing these cells in vitro, researchers can recreate the tumor microenvironment and study the effects of various therapeutic agents on cancer cell proliferation, migration, and invasion. This approach allows for the identification of promising drug candidates and the optimization of treatment strategies, ultimately paving the way for more effective and personalized cancer therapies.
Biomarker discovery and diagnostics
Colorectal tumor cells also serve as valuable tools for the discovery and development of biomarkers, which are molecules or characteristics that can be used to detect, monitor, and even predict the course of the disease. By analyzing the unique molecular signatures and cellular behaviors of these tumor cells, scientists have identified novel biomarkers that can aid in early cancer detection, risk stratification, and treatment selection.
Tumor microenvironment and immune interactions
Furthermore, research has delved into the intricate interplay between colorectal tumor cells and the surrounding tumor microenvironment. The role of various cellular and non-cellular components, such as immune cells, stromal cells, and extracellular matrix, in shaping the tumor's immune landscape and response to treatment. These insights have enabled us to explore novel immunotherapeutic strategies that harness the body's immune system to combat colorectal cancer.
Interference With Notch3 Signalling Attenuates Colon Tumour Growth
Macrophage infiltration in the tumor microenvironment participates in the regulation of tumor progression. Previous studies have found that the Notch signaling pathway is involved in regulating the progression of colorectal cancer (CRC), however, the specific mechanism is still unclear.
To test whether Notch3 was involved in regulating the recruitment of macrophages in vivo, an MC38 cell line with stable knockdown of Notch3 was constructed (Fig. 1a). The colony formation assay showed that interference with Notch3 expression in vitro had little effect on cell proliferation (Fig. 1b), which was also verified in 3D growth of MC38 cells (Fig. 1c). Next, control and Notch3 stable knockdown MC38 cells were injected on both sides of C57BL/6 mice. Surprisingly, interference with Notch3 significantly inhibited the growth of transplanted tumors (Fig. 1d-f). The above results indicated that Notch3 mainly promoted the development of CRC by regulating the tumor microenvironment. Furthermore, a flow cytometry experiment was conducted to detect macrophage in the tumor microenvironment of transplanted tumors. The results showed that interference with Notch3 significantly reduced the proportion of macrophage in tumor tissues (Fig. 1g, h). Meanwhile, the proportion of macrophage was analyzed in the peripheral blood of mice, and no significant changes were observed. Altogether, the results suggested that Notch3 participated in regulating the recruitment of macrophages in colon cancer, thereby regulating tumor progression.
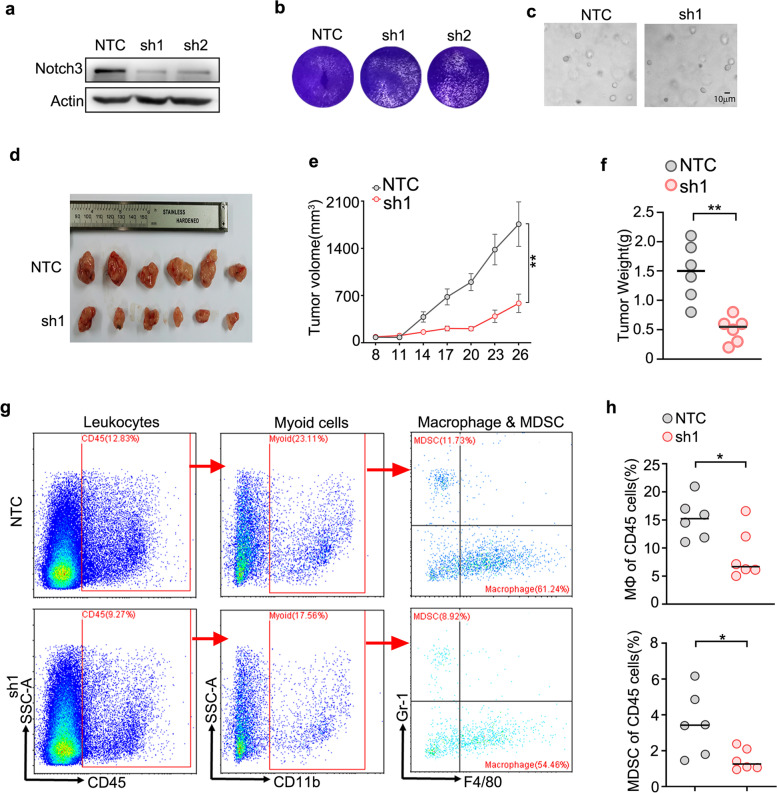 Fig.
1 Interference Notch3 attenuates the colon tumor growth and decreases Macrophage infiltration in vivo.
(Huang K, et al, 2023)
Fig.
1 Interference Notch3 attenuates the colon tumor growth and decreases Macrophage infiltration in vivo.
(Huang K, et al, 2023)
Effect of IFN-γ Stimulation on the Proliferation of CRC Cells
Interferon-γ (IFN-γ), also called immune interferon, is an important cytokine present in the tumor microenvironment (TME). In addition to playing a role in the defense against infection, IFN-γ also plays a prominent role in tumor diseases.
In the in vitro study, the proliferation of three CRC cell lines, CT26.WT, DLD-1, and SW480 were evaluated before and after IFN-γ stimulation using Cell Counting Kit-8 (CCK-8) assays and found that the absorbance value showed a decreasing trend in the IFN-γ stimulation group compared with the control group (without cytokine stimulation). These results showed that IFN-γ stimulation inhibited tumor cell proliferation in vitro (Fig. 2A).
In the in vivo study, IM-d-mice and IM-c-mice were selected for tumor growth assays using implanted CRC cells. First, the growth trend of subcutaneously implanted CT26.WT tumors were examined in IM-d mice. The IFN-γ stimulation group was compared with the control group, and the curves of both tumor volume (Fig. 2B) and final tumor weight (Fig. 2C) showed a decreasing trend in the IFN-γ stimulation group. These results suggest that IFN-γ stimulation can inhibit tumor growth in IM-d-mice, which is consistent with the results of the in vitro CCK-8 assay. However, in IM-c-mice, the tumors in IFN-γ-stimulated mice grew faster, and the final tumor volume (Fig. 2D) and weight were larger (Fig. 2E) than those in control mice. These results showed that IFN-γ stimulation promoted CRC tumor growth in IM-c mice. Therefore, IFN-γ may exert an immunomodulatory effect through the TME.
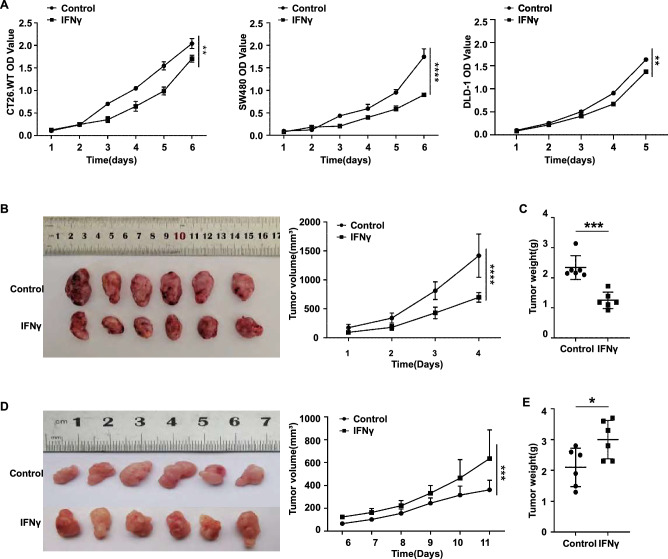 Fig.
2 IFN-γ stimulation of CRC cell proliferation depends on the immune microenvironment. (Jing ZL, et al.,
2024)
Fig.
2 IFN-γ stimulation of CRC cell proliferation depends on the immune microenvironment. (Jing ZL, et al.,
2024)
The primary differences between colorectal tumor cells and normal colonic epithelial cells lie in their proliferative capacity, genomic stability, and signaling pathways.
Colorectal tumor cells have dysregulated signaling pathways, such as the Wnt, EGFR, and PI3K/Akt pathways, which promote their survival, invasion, and metastasis, in contrast to the tightly regulated signaling in normal colonic epithelial cells.
While colorectal tumor cell models are invaluable research tools, they do have some limitations including genetic instability, lack of tumor heterogeneity, absence of tumor microenvironment, and differences in metabolic profiles.
Filters Clear all filters
Species
- African clawed frog (1)
- American mink (1)
- Asian tiger mosquito (1)
- Atlantic salmon (1)
- Bluegill (2)
- Bluestriped grunt (1)
- Bovine (7)
- Brazilian free-tailed bat (1)
- Brown bullhead (2)
- Cabbage looper (1)
- Cabbage moth (6)
- Cat (4)
- Central mudminnow (1)
- Chicken (3)
- Chinese hamster (5)
- Chinook salmon (2)
- Chum salmon (1)
- Coho salmon (1)
- Common carp (2)
- Cotton-top tamarin (1)
- Dog (2)
- Fall armyworm (3)
- Fathead minnow (2)
- Fruit fly (1)
- Gilthead sea bream (2)
- Golden hamster (7)
- Goldfish (6)
- Gray dwarf hamster (1)
- Green monkey (2)
- Gypsy moth (1)
- Horse (1)
- Human (999)
- Japanese eel (1)
- Japanese rice fish (7)
- Koi carp (1)
- Mouse (315)
- Mouse x Gray dwarf hamster (1)
- Mouse x Rat (20)
- Northern pike (1)
- Pig (3)
- Rabbit (2)
- Rainbow trout (3)
- Rat (115)
- Rhesus macaque (1)
- Salt marsh moth (1)
- Sheep (2)
- Snakehead murrel (2)
- Sockeye salmon (1)
- Vervet monkey (2)
- Zebrafish (2)
Source
- Abdomen (1)
- Abdomen Metastasis (2)
- Adipose (2)
- Adrenal Gland (8)
- Adrenal Gland Metastasis (2)
- Aorta (4)
- Artery (1)
- Ascites (28)
- Ascites Metastasis (37)
- Bile Duct (3)
- Bladder (25)
- Bladder Metastasis (1)
- Blastocyst (1)
- Blastula (1)
- Blood (127)
- Bone (27)
- Bone Marrow (57)
- Bone Marrow Metastasis (18)
- Bone Metastasis (6)
- Brain (55)
- Brain Metastasis (8)
- Breast (30)
- Bronchus (1)
- Caudal Peduncle (1)
- Caudal Trunk (2)
- Cecum (3)
- Cerebrospinal Fluid (1)
- Cerebrospinal Fluid Metastasis (1)
- Cervix (32)
- Colon (90)
- Connective Tissue (7)
- Cornea (3)
- Cutaneous Metastasis (1)
- Dermis (2)
- Duodenum (1)
- Embryo (29)
- Endometrium (17)
- Esophagus (44)
- Eye (12)
- Eye Socket (5)
- Fetus (3)
- Fin (9)
- Foreskin (4)
- Gallbladder (1)
- Gingiva (2)
- Globe (2)
- Glomerulus (2)
- Groin (1)
- Head Kidney (2)
- Heart (4)
- Hemolymph (1)
- Hypodermis Metastasis (5)
- Ileum (1)
- Intestine (94)
- Jejunum (1)
- kidney (1)
- Kidney (27)
- Liver (35)
- Liver Metastasis (17)
- Lung (58)
- Lung Metastasis (8)
- Lymph Node (8)
- Lymph Node Metastasis (59)
- Muscle (7)
- Muscle Metastasis (2)
- Nose (2)
- Omentum Metastasis (2)
- Oral Cavity (10)
- Ovary (21)
- Ovary Metastasis (2)
- Pancreas (19)
- Pelvic Wall Metastasis (1)
- Pelvis (1)
- Perianal Space Metastasis (1)
- Pericardial Effusion (1)
- Pericardial Effusion Metastasis (2)
- Perineus (1)
- Peripheral Blood (126)
- Peripheral Nervous System (21)
- Peritoneal Effusion (2)
- Peritoneum (1)
- Peritoneum Metastasis (1)
- Pharynx (3)
- Pituitary Gland (7)
- Pleural Effusion (54)
- Pleural Effusion Metastasis (46)
- Prostate (7)
- Rectum (15)
- Renal Pelvis (1)
- Retroperitoneal Space (2)
- Salivary Gland (2)
- Skeletal Muscle (5)
- Skin (32)
- Skin Metastasis (3)
- Small Intestine (4)
- Small Intestine Metastasis (1)
- Smooth Muscle (2)
- Soft Tissue (1)
- Soft Tissue Metastasis (1)
- Spinal Cord (2)
- Stomach (4)
- Testis (15)
- Thoracic Cavity Metastasis (6)
- Thymus (5)
- Thyroid Gland (16)
- Thyroid Gland Metastasis (1)
- Tongue (5)
- Trachea (1)
- Umbilical Cord (1)
- Umbilical Cord Blood (1)
- Urachus (1)
- Ureter (1)
- Uterus (54)
- Uvea (2)
- Vagina (2)
- Vulva (1)
Disease
- Acute Biphenotypic Leukemia (1)
- Acute Erythroid Leukemia (4)
- Acute Megakaryoblastic Leukemia (4)
- Acute Monocytic Leukemia (9)
- Acute Myeloid Leukemia (25)
- Acute Promyelocytic Leukemia (2)
- Adrenal Gland Neuroblastoma (11)
- Adult B Acute Lymphoblastic leukemia (1)
- Adult B Acute Lymphoblastic Leukemia (6)
- Adult T Acute Lymphoblastic Leukemia (6)
- Adult T Lymphoblastic Lymphoma (2)
- Adult T-Cell Leukemia/Lymphoma (1)
- Alveolar Rhabdomyosarcoma (4)
- Alveolar Ridge Squamous Cell Carcinoma (1)
- Amelanotic Melanoma (3)
- Ampulla of Vater Adenocarcinoma (1)
- Ampulla of Vater Adenosquamous Carcinoma (3)
- Anaplastic Astrocytoma (3)
- Anaplastic Large Cell Lymphoma (7)
- Askin Tumor (1)
- Astrocytoma (5)
- B Acute Lymphoblastic Leukemia (2)
- B-Cell Non-Hodgkin Lymphoma (5)
- Bare Lymphocyte Syndrome Type 2 (1)
- Barrett Adenocarcinoma (2)
- Benign Prostatic Hyperplasia (1)
- Bladder Carcinoma (14)
- Bladder Squamous Cell Carcinoma (1)
- Bovine Leukemia (2)
- Breast Adenocarcinoma (4)
- Breast Carcinoma (9)
- Breast Ductal Carcinoma (2)
- Burkitt Lymphoma (17)
- Canavan Disease (1)
- Canine Histiocytic Sarcoma (1)
- Cecum Adenocarcinoma (3)
- Central Nervous System Lymphoma (2)
- Cervical Adenocarcinoma (2)
- Cervical Adenosquamous Carcinoma (2)
- Cervical Small Cell Carcinoma (1)
- Cervical Squamous Cell Carcinoma (2)
- Chicken Bursal Lymphoma (2)
- Childhood B Acute Lymphoblastic Leukemia (13)
- Childhood T Acute Lymphoblastic Leukemia (16)
- Childhood T Lymphoblastic Lymphoma (1)
- Cholangiocarcinoma (2)
- Chronic Eosinophilic Leukemia (1)
- Chronic Lymphocytic Leukemia (2)
- Chronic Myeloid Leukemia (23)
- Clear Cell Renal Cell Carcinoma (2)
- Colon Adenocarcinoma (55)
- Colon Carcinoma (34)
- Colorectal Adenocarcinoma (1)
- Colorectal Carcinoma (1)
- Congenital Pure Red Cell Aplasia (1)
- Cutaneous Melanoma (10)
- Dedifferentiated Chondrosarcoma (1)
- Desmoplastic Melanoma (1)
- Diffuse Large B-Cell Lymphoma (29)
- Down Syndrome (2)
- EBV-Related Burkitt Lymphoma (12)
- Embryonal Carcinoma (3)
- Embryonal Rhabdomyosarcoma (3)
- Endometrial Adenocarcinoma (13)
- Endometrial Adenosquamous Carcinoma (2)
- Endometrial Carcinoma (2)
- Endometrioid Stromal Sarcoma (1)
- Epithelioid Hemangioendothelioma (1)
- Epithelioid Sarcoma (3)
- Esophageal Adenocarcinoma (6)
- Esophageal Squamous Cell Carcinoma (41)
- Essential Thrombocythemia (1)
- Ewing Sarcoma (2)
- Extraskeletal Myxoid Chondrosarcoma (1)
- Fanconi Anemia (1)
- Fibrosarcoma (1)
- Follicular Lymphoma (2)
- Gallbladder Carcinoma (2)
- Gallbladder Undifferentiated Carcinoma (2)
- Gastric Adenocarcinoma (6)
- Gastric Adenosquamous Carcinoma (1)
- Gastric Carcinoma (5)
- Gastric Choriocarcinoma (1)
- Gastric Fundus Carcinoma (1)
- Gastric Signet Ring Cell Adenocarcinoma (1)
- Gastric Small Cell Carcinoma (2)
- Gastric Tubular Adenocarcinoma (5)
- Gastroesophageal Junction Adenocarcinoma (1)
- Gestational Choriocarcinoma (1)
- Gingival Squamous Cell Carcinoma (2)
- Glioblastoma (18)
- Gliosarcoma (1)
- Goldfish Erythrophoroma (4)
- Hairy Cell Leukemia (1)
- Hamster Kidney Tumor (1)
- Hamster Pancreatic Ductal Adenocarcinoma (1)
- Hamster Uterine Leiomyosarcoma (1)
- Hepatoblastoma (2)
- Hepatocellular Carcinoma (6)
- Hepatosplenic T-Cell Lymphoma (2)
- Hereditary Thyroid Gland Medullary Carcinoma (1)
- High Grade B-Cell Lymphoma (1)
- High Grade Ovarian Serous Adenocarcinoma (8)
- Hodgkin Lymphoma (9)
- Hypopharyngeal Squamous Cell Carcinoma (2)
- Infectious Mononucleosis (1)
- Intrahepatic Cholangiocarcinoma (6)
- Invasive Breast Carcinoma of No Special Type (12)
- Invasive Breast Lobular Carcinoma (1)
- Kidney Neoplasm (1)
- Kidney Rhabdoid Tumor (1)
- Krukenberg Tumor (1)
- Liposarcoma (1)
- Lung Adenocarcinoma (17)
- Lung Giant Cell Carcinoma (8)
- Lung Large Cell Carcinoma (9)
- Lung Mucoepidermoid Carcinoma (1)
- Lung Non-Small Cell Carcinoma (2)
- Lung Small Cell Carcinoma (25)
- Lung Squamous Cell Carcinoma (9)
- Lymphoblastic Lymphoma (1)
- Malignant Peripheral Nerve Sheath Tumor (1)
- Mantle Cell Lymphoma (5)
- Mature Gastric Teratoma (1)
- Maxillary Sinus Squamous Cell Carcinoma (1)
- Medaka Hepatoma (2)
- Medulloblastoma (3)
- Melanoma (24)
- Meningioma (2)
- Minimally Invasive Lung Adenocarcinoma (1)
- Monophasic Synovial Sarcoma (1)
- Mouse Bladder Transitional Cell Carcinoma (1)
- Mouse Chondrosarcoma (1)
- Mouse Colon Adenocarcinoma (3)
- Mouse Ependymoma (2)
- Mouse Erythroid Leukemia (13)
- Mouse Fibrosarcoma (5)
- Mouse Glioblastoma (1)
- Mouse Hemangioendothelioma (1)
- Mouse Hepatocellular Carcinoma (1)
- Mouse Insulinoma (3)
- Mouse Intestinal Tract Neuroendocrine Adenoma (1)
- Mouse Islet Cell Adenoma (1)
- Mouse Kidney Carcinoma (1)
- Mouse Leukemia (10)
- Mouse Leydig Cell Tumor (1)
- Mouse Lymphoma (8)
- Mouse Mammary Gland Malignant Neoplasm (23)
- Mouse Melanoma (9)
- Mouse Multiple Myeloma (5)
- Mouse Myeloid Leukemia (3)
- Mouse Neoplasm (1)
- Mouse Neuroblastoma (21)
- Mouse Oral Cavity Squamous Cell Carcinoma (1)
- Mouse Osteosarcoma (3)
- Mouse Pituitary Gland Neoplasm (1)
- Mouse Plasmacytoma (1)
- Mouse Precursor T Cell Lymphoblastic Lymphoma/Leukemia (2)
- Mouse Pulmonary Adenoma (1)
- Mouse Pulmonary Malignant Tumor (3)
- Mouse Pulmonary Squamous Cell Carcinoma (1)
- Mouse Rectum Carcinoma (2)
- Mouse Reticulum Cell Sarcoma (2)
- Mouse Sarcoma (1)
- Mouse Teratocarcinoma (8)
- Mouse Thymic Lymphoma (3)
- Mycosis Fungoides (1)
- Myelodysplastic Syndrome (1)
- Myxofibrosarcoma (1)
- Natural Killer Cell Lymphoblastic Leukemia/Lymphoma (2)
- Neuroblastoma (26)
- Oral Cavity Squamous Cell Carcinoma (15)
- Osteoid Osteoma (1)
- Osteosarcoma (15)
- Ovarian Carcinoma (1)
- Ovarian Clear Cell Adenocarcinoma (1)
- Ovarian Endometrioid Adenocarcinoma (4)
- Ovarian Granulosa Cell Tumor (1)
- Ovarian Mucinous Adenocarcinoma (2)
- Ovarian Serous Adenocarcinoma (2)
- Ovarian Serous Cystadenocarcinoma (2)
- Ovarian Small Cell Carcinoma (1)
- Pancreatic Adenocarcinoma (13)
- Pancreatic Carcinoma (5)
- Pancreatic Ductal Adenocarcinoma (12)
- Papillomavirus-Independent Cervical Squamous Cell Carcinoma (1)
- Papillomavirus-Related Cervical Adenocarcinoma (7)
- Papillomavirus-Related Cervical Squamous Cell Carcinoma (4)
- Papillomavirus-Related Endocervical Adenocarcinoma (16)
- Paroxysmal Nocturnal Hemoglobinuria (3)
- Pharyngeal Squamous Cell Carcinoma (1)
- Plasma Cell Myeloma (15)
- Pleural Epithelioid Mesothelioma (5)
- Pleural Sarcomatoid Mesothelioma (2)
- Poorly Differentiated Thyroid Gland Carcinoma (1)
- Primary Cutaneous T-Cell Non-Hodgkin Lymphoma (1)
- Primary Effusion Lymphoma (7)
- Primitive Neuroectodermal Tumor (1)
- Prostate carcinoma (1)
- Prostate Carcinoma (9)
- Rat C-Cell Carcinoma (1)
- Rat Cholangiocarcinoma (1)
- Rat Colon Adenocarcinoma (5)
- Rat Digestive System Neoplasm (1)
- Rat Fibrosarcoma (1)
- Rat Hepatocellular Carcinoma (20)
- Rat Histiocytic Sarcoma (1)
- Rat Insulinoma (2)
- Rat Leukemia (1)
- Rat Leydig Cell Adenoma (1)
- Rat Lung Carcinoma (1)
- Rat Malignant Glioma (4)
- Rat Malignant Meningioma (1)
- Rat Malignant Oligodendroglioma (2)
- Rat Malignant Thymoma (3)
- Rat Mammary Gland Adenocarcinoma (10)
- Rat Neuroblastoma (3)
- Rat Osteosarcoma (2)
- Rat Pituitary Gland Neoplasm (6)
- Rat Prostate Adenocarcinoma (3)
- Rat Rhabdomyosarcoma (1)
- Rat Sarcoma (2)
- Rat Squamous Cell Carcinoma (1)
- Rat Urinary Bladder Transitional Cell Carcinoma (2)
- Rat Urinary System Neoplasm (6)
- Rectal Adenocarcinoma (13)
- Rectosigmoid Adenocarcinoma (1)
- Recurrent Bladder Carcinoma (1)
- Renal Cell Carcinoma (7)
- Renal Pelvis Urothelial Carcinoma (1)
- Retinoblastoma (11)
- Sacral Chordoma (1)
- Sacrococcygeal Teratoma (1)
- Salivary Gland Squamous Cell Carcinoma (1)
- Sezary Syndrome (1)
- Shwachman-Diamond Syndrome (1)
- Skin Squamous Cell Carcinoma (2)
- Splenic Marginal Zone Lymphoma (1)
- Testicular Embryonal Carcinoma (8)
- Testicular Teratoma (2)
- Testicular Yolk Sac Tumor (1)
- Thyroid Gland Anaplastic Carcinoma (10)
- Thyroid Gland Follicular Carcinoma (4)
- Thyroid Gland Papillary Carcinoma (3)
- Thyroid Gland Sarcoma (1)
- Thyroid Gland Squamous Cell Carcinoma (2)
- Tongue Adenosquamous Carcinoma (1)
- Tongue Squamous Cell Carcinoma (6)
- Type I Endometrial Adenocarcinoma (1)
- Ureter Urothelial Carcinoma (1)
- Uterine Carcinosarcoma (2)
- Uterine Corpus Leiomyosarcoma (1)
- Uterine Corpus Sarcoma (2)
- Uveal Melanoma (2)
- Vaginal Melanoma (2)
- Vulvar Melanoma (1)
- Vulvar Squamous Cell Carcinoma (1)
Description: The Adriamycin-resistant cell line HCT8/ADR has been developed by repeatedly exposing the parent ...
Description: The Fluorouracil-resistant cell line HCT8/5FU has been developed by repeatedly exposing the parent ...
Description: The Oxaliplatin-resistant cell line HCT8/L-OHP has been developed by repeatedly exposing the parent ...
Description: The Paclitaxel-resistant cell line HCT-15/taxol has been developed by repeatedly exposing the ...
Description: Species: human, Caucasian male 53 years old; Tissue: rectum; Tumor: adenocarcinoma, grade IV
Description: Established from the ascites fluid of a 71-year-old man with colon carcinoma in 1975; The cell line ...
Description: Established from the tumor mass of a 55-year-old Caucasian woman with a moderately undifferentiated ...
Description: Established from a colorectal adenocarcinoma; HCT-15 is a sister cell line of the cell line DLD-1. ...
Description: The Fluorouracil-resistant cell line HCT-15/5FU has been developed by repeatedly exposing the ...
Description: The Paclitaxel-resistant cell line HCT-8/taxol has been developed by repeatedly exposing the parent ...
Description: Established from the primary tumor at the left colon (a moderately differentiated colorectal ...
Description: Established from a male patient with a well-differentiated primary sigmoid adenocarcinoma of TNM ...
Description: Established from a woman with a moderately differentiated primary adenocarcinoma of the right colon ...
Description: Established from the primary colorectal cancer (TNM stage 3) of the right colon of a woman; cells ...
Description: Established from the primary colon carcinoma of an adult man; cells were described to carry a RAS ...
Description: The Cisplatin-resistant cell line HCT-116/DDP has been developed by repeatedly exposing the parent ...
Description: The Onvansertib-resistant cell line HCT-116/Onv has been developed by repeatedly exposing the ...
Description: Subline of H414 cell line lacking MDC1 gene in both alleles.