
Human iPSC-Derived Cardiomyocytes
Cat.No.: CSC-C2847SC
Species: Human
Cell Type: Cardiomyocyte
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Over the last decade, heart failure has been the leading cause of death across the world. Since cardiomyocytes are terminally differentiated with a limited capacity for division, and the adult heart lacks effective repair mechanisms, cell-based regenerative therapy has become a novel therapeutic paradigm for myocardial repair. iPSC-derived cardiomyocytes (iPSC-CMs) have been widely touted to have tremendous potential for repairing damaged heart tissue due to the large-scale production of human iPSC-derived cardiomyocytes (hiPSC-CMs), providing a reliable source of cells for cardiac muscle transplants. Additionally, there have been relatively few new drugs in the market for the treatment of heart disease. A major challenge in developing new drugs for heart disease is that positive results from preclinical studies are often contradicted by discouraging outcomes from larger trials. A potential explanation for the challenges of developing new cardiovascular disease (CVD) drugs is the lack of a suitable platform to screen for novel therapeutic strategies. In the last decade, drug toxicity and disease modeling have relied heavily on animal models, which have serious shortcomings. Differences in pathophysiology, drug metabolism, and species-specific gene expression between humans and animals hinder the generalization of potential drugs' efficacy and toxicity from animal models to clinical patients. HiPSCs can provide researchers with a limitless number of disease-relevant cells and allow us to mimic the in vivo environment of a human.
In Vitro Models
The use of iPSC-CMs in cardiovascular research has attracted much attention because they have similar properties to CMs in vitro, including many drug-affected targets and disease-associated genetic mutations, making it possible to use these cells for drug screening with or without inducing specific disease phenotypes, as well as exploring the pathological mechanisms of heart disease.
In the absence of specific induced phenotypes, iPSC-CMs can serve as a preclinical cardiac platform for screening the cardiotoxicity of drug candidates. In particular, rare drug-induced fatal ventricular arrhythmia, such as torsades de pointes (TdP), is the focus of cardiac safety in current regulatory guidelines.
In addition to cardiac disease models, iPSC-CMs are potential platforms for drug toxicity models, especially chemotherapy-induced cardiotoxicity. Chemotherapy-induced cardiac dysfunction can be recapitulated by hiPSC-CMs at a single-cell level.
Regenerative Engineering
Currently, there are two main effective strategies for treating heart failure, heart transplantation and ventricular assist devices. However, the development of myocardial infarction (MI) treatments is usually limited by many issues including donor organ shortage, immunological rejection, and invasive surgery. Recently, autologous transplantation of iPSC-CMs has been widely considered as a promising alternative strategy compared with other cell sources because it excludes the possibility of immune rejection.
Heart-on-a-Chip
Heart-on-a-chip, also known as microphysiological system, has emerged as a promising candidate for screening for cardiac safety and efficacy. The heart-on-a-chip is an innovative multidiscipline 3D cardiac tissue fabrication method for replicating cardiac tissue. Microsystem engineering allows researchers to develop a microphysiological environment composed of cardiac cells that recapitulate cardiac tissue or organ structure and function in vitro, with the advantage of requiring fewer cells and greater reproducibility.
iPSC-CMs based heart-on-a-chip is widely recognized as a miniaturized 3D cardiac tissue and heart model. However, before iPSC-CM based heart-on-a-chip becomes a useful method for drug discovery in the industry, there are still some challenges that need to be addressed beforehand, such as the lack of large-scale production, continuous and automated processes, as well as quality control during the manufacturing process.
Flow Cytometry and Immunofluorescence Analysis of hiPSC-CMs
Figure 1A shows representative flow cytometry data to assess cardiomyocyte purity. "Live" (live/dead stain) permeabilized cardiomyocytes were stained for cTNT or matching isotype control. For each analysis, the cardiomyocyte cultures contained cTNT-positive cells with a purity of >98%, and after 2 week in culture, cardiomyocyte purity remained unchanged. Figure 1B shows a cardiomyocyte monolayer immunostained for sarcomeric α-actinin (red) and nuclei (blue). Nuclei are evenly distributed and α-actinin staining is present throughout the field. The higher power image (inset) shows the subcellular sarcomeric organization of contractile myofibrils.
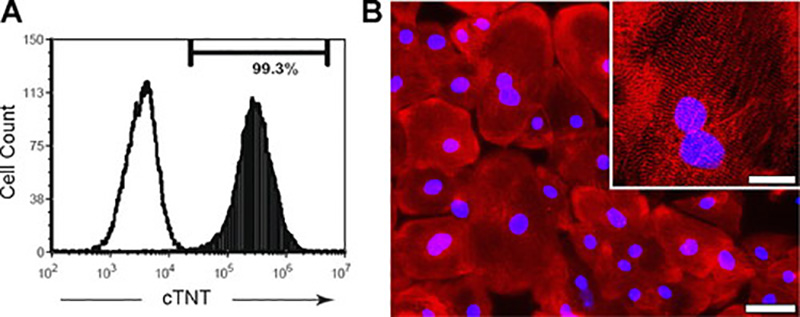 Fig. 1. Purity and structure of cardiomyocytes (Ma, Junyi, et al., 2011).
Fig. 1. Purity and structure of cardiomyocytes (Ma, Junyi, et al., 2011).
Action Potentials (APs) Properties of hiPSC-CMs
APs from 59 cardiomyocytes that beat spontaneously at a constant rate were analyzed for beat rate interval (Interval), maximum diastolic potential (MDP), peak voltage (Peak), amplitude (Amp), maximal rate of depolarization (dV/dtmax), and AP duration (APD) at different levels of repolarization (APD measured at 10% increments of Amp). These data are summarized in Fig. 2. The following criteria were used to distinguish the AP phenotypes: atrial- and ventricular-like APs displayed more negative MDPs with higher dV/dtmax values and larger amplitudes than nodal-like APs. Ventricular-like APs have a distinct plateau phase (phase 2) after which repolarization accelerates (phase 3). This was measured as the time difference between APD30 to APD40 (APD30-40) and the time difference between APD70 to APD80 (APD70-80). Ventricular-like APs had a ratio (APD30-40/APD70-80) of ∼2.5 compared with the atrial-like ratio of ∼1.1, thus, APs with a ratio >1.5 were categorized as ventricular like. Ventricular-like APs had longer duration APDs with slower rates of spontaneous beating (increased Interval), whereas atrial-like APs had a minimal plateau phase (APD30-40/APD70-80 close to unity) with shorter durations and higher spontaneous beating rates. Nodal-like APs had less negative MDPs and smaller amplitudes with lower dV/dtmax values (<10 V/s). With the use of these criteria, 54% of the 59 cardiomyocytes displayed ventricular-like APs, 22% showed nodal-like APs, and 24% showed atrial-like APs.
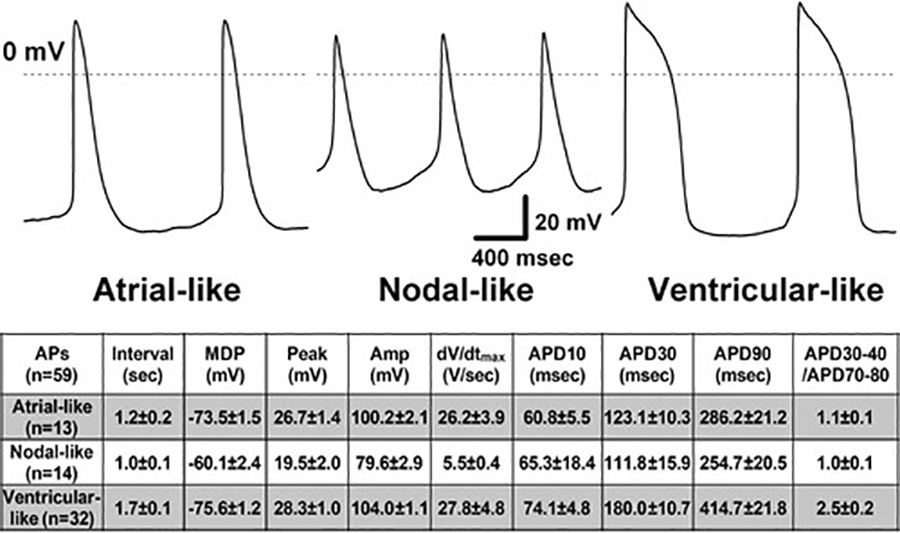 Fig. 2. Action potentials (APs) were recorded from hiPSC-CMs at 35-37°C using the perforated patch-clamp method (Ma, Junyi, et al., 2011).
Fig. 2. Action potentials (APs) were recorded from hiPSC-CMs at 35-37°C using the perforated patch-clamp method (Ma, Junyi, et al., 2011).
The effects of selective ion channel block were tested on cardiomyocytes with ventricular-like AP waveforms stimulated at a constant rate of 1 Hz. For control experiments, AP parameters were stable over a 15-min recording period in extracellular solution without (Fig. 3A, left) or containing 0.1% DMSO (Fig. 3B, left). Selective block of INa by TTX had no effect on AP parameters at 1 μmol/L, whereas increasing concentrations (3-30 μmol/L) delayed the upstroke and reduced dV/dtmax (Fig. 3A, middle). Selective block of the IKr by E4031 caused concentration-dependent (3-100 nmol/L) slowing of repolarization to "triangulate" the AP (Fig. 3A, right). Selective block of ICa by nifedipine caused concentration-dependent (3-100 nmol/L) shortening of the AP throughout repolarization with minimal effects on the AP peak voltage and dV/dtmax (Fig. 3B, middle). Suppression of the IKs by 3R4S-chromanol 293B had minimal effects on AP properties up to 10 μmol/L sufficient to cause >50% block of IKs (Fig. 3B, right). For measurements of APD, the time of dV/dtmax was used as the start time for the AP. TTX caused slowing of dV/dtmax, E4031 caused lengthening of APD50 and APD90, and nifedipine caused shortening of APD10, APD50, and APD90. Single EADs were induced by 30-100 nmol/L E4031 in three of five cardiomyocytes paced at 0.5 Hz. Figure 3C shows that lower concentrations of E4031 prolonged the AP and that 100 nmol/L induced single EADs. Similar to cardiac myocytes, EADs in hiPSC-derived cardiomyocytes were rate dependent and disappeared upon increasing the pacing rate from 0.5 to 1 Hz. Furthermore, there was an inverse relation between the EAD peak voltage and EAD take-off potential, as is shown in Fig. 3D for 79 single EADs from the same cardiomyocyte (inset shows 2 EADs with differing amplitudes and take-off potentials).
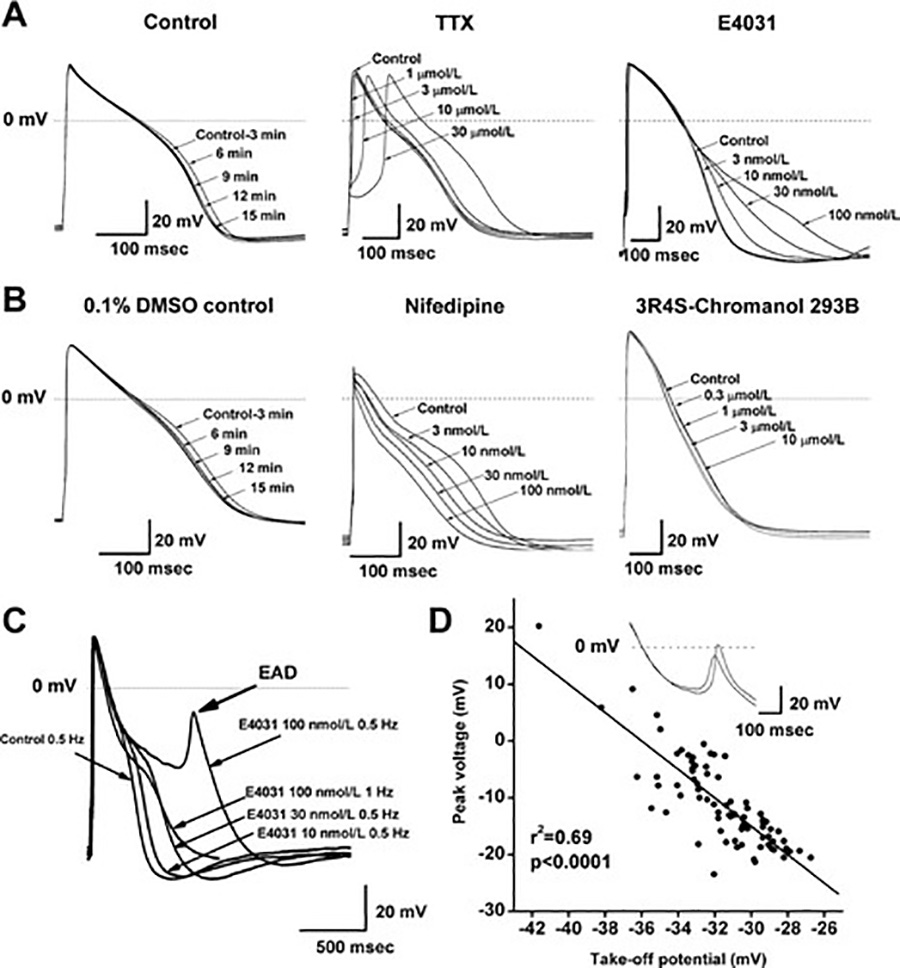 Fig. 3. Effects of ion channel blocking drugs on AP morphology. Data were recorded at 35–37°C with the perforated patch-clamp method (Ma, Junyi, et al., 2011).
Fig. 3. Effects of ion channel blocking drugs on AP morphology. Data were recorded at 35–37°C with the perforated patch-clamp method (Ma, Junyi, et al., 2011).
To generate hiPSC-derived cardiomyocytes, adult cells, such as skin cells or blood cells, are reprogrammed into induced pluripotent stem cells. These iPSCs are then differentiated into cardiomyocytes through a series of steps that mimic heart development in the human body.
hiPSC-derived cardiomyocytes are used in drug development to screen for potential cardiac toxicity of new drugs, to study the mechanisms of cardiovascular diseases, and to test the efficacy of novel therapeutic compounds targeting heart diseases.
Some challenges of using hiPSC-derived cardiomyocytes include variability in differentiation efficiency, maturation level, and functional properties among batches of cells, as well as the need to improve the scalability, reproducibility, and standardization of current differentiation protocols.
Ask a Question
Average Rating: 5.0 | 1 Scientist has reviewed this product
Excellent viability and functionality
I recently purchased Human iPSC-Derived Cardiomyocytes from Creative Bioarray and I have been extremely pleased with this product. The cardiomyocytes arrived frozen and were easy to thaw and culture. They have displayed excellent viability and functionality in my experiments, consistently beating in a synchronized manner. I have been able to obtain reliable and reproducible data using these cells, and I would highly recommend these cardiomyocytes to anyone looking for a high-quality cell model for cardiac research.
06 Dec 2023
Ease of use
After sales services
Value for money
Write your own review
- You May Also Need
