
Human Bronchial Smooth Muscle Cells (HBSM)
Cat.No.: CSC-7821W
Species: Human
Source: Bronchus
Cell Type: Smooth Muscle Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Airway smooth muscle is fundamental for maintaining airway tone. The specialized ultrastructural features and regulatory mechanisms of airway smooth muscle are vital for normal airway function. Patients with respiratory disorders, such as severe asthma, exhibit the distinguishing feature of increased bronchial smooth muscle mass. The increase in smooth muscle mass is related either to abnormal bronchial smooth muscle cell (BSMC) proliferation or the accumulation of contractile protein. Smooth muscle cell proliferation is an important component of airway remodeling in asthma. It is consequently a target for the development of novel anti-asthma agents. Airway smooth muscle cells express CT-1 and release GM-CSF, RANTES and IL-8 in vitro. In order to develop therapies for asthma, researchers have utilized Human Bronchial Smooth Muscle Cells to elucidate the cellular and molecular mechanisms underlying BSMC proliferation.
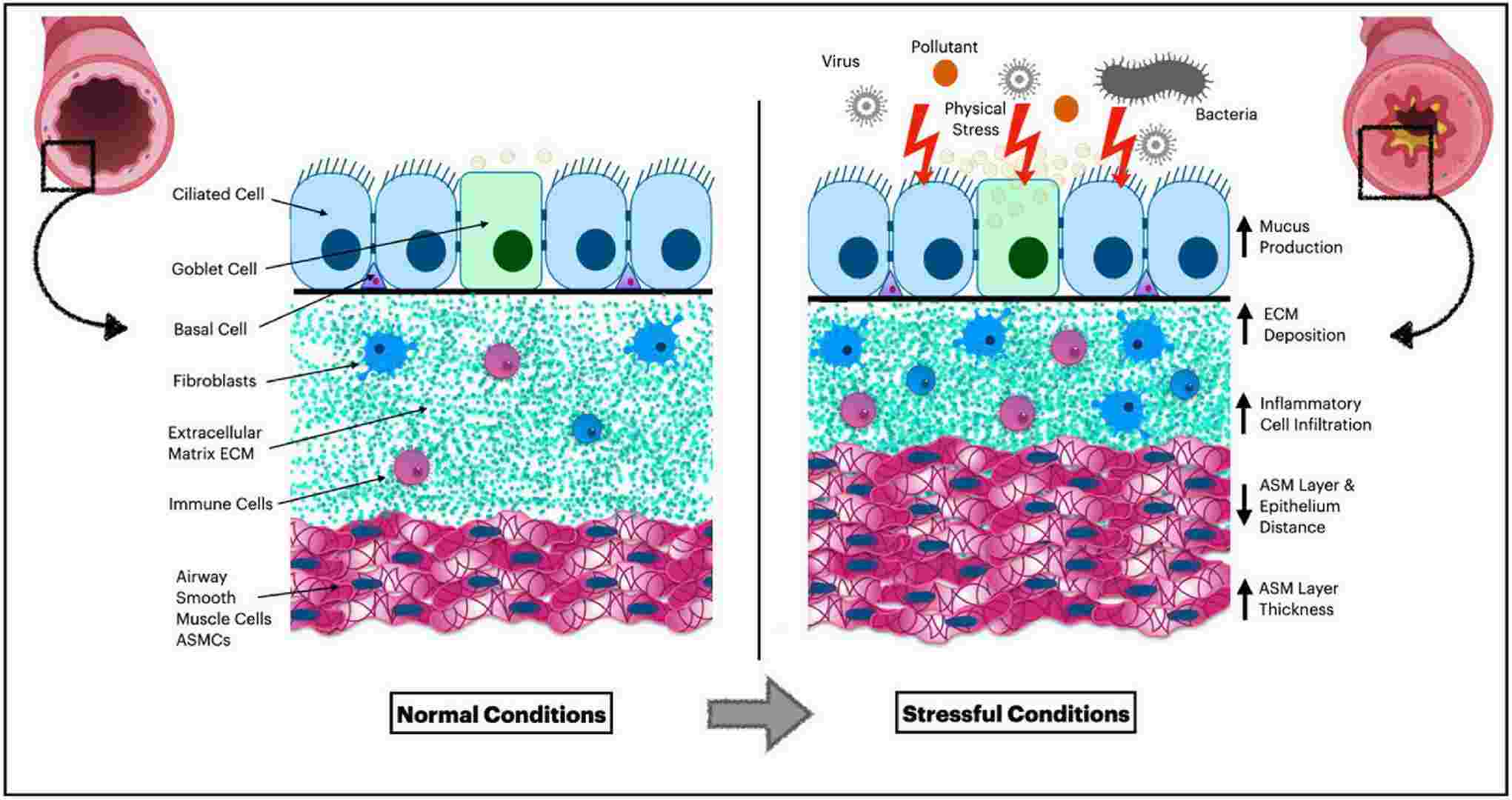 Fig. 1. Airway cellular pathophysiology (Abohalaka, Reshed. 2023).
Fig. 1. Airway cellular pathophysiology (Abohalaka, Reshed. 2023).
Creative Bioarray provides high quality Human Bronchial Smooth Muscle Cells (HBSMC), which are isolated from human bronchi and bronchioles and cryopreserved at P2, with >0.5 million cells in each vial. HBSMC express α-smooth muscle actin and desmin and are negative for HIV-1, HBV, HCV, mycoplasma, bacteria, yeast, and fung. HBSMC can further expand in Smooth Muscle Cell Growth Medium (Cat# CM-1194W) under the condition suggested by Creative Bioarray.
Diseased Human Bronchial Smooth Muscle Cells are also available from donors diagnosed with asthma, COPD and cystic fibrosis. Detailed donor information for these cells can be obtained by contacting our scientific support team.
Zedoarondiol Inhibits Human Bronchial Smooth Muscle Cell Proliferation Through the CAV-1/PDGF Signaling Pathway
Airway remodeling in lung diseases can be treated by inhibiting excessive smooth muscle cell proliferation. Zedoarondiol (Zed) is a natural compound isolated from the Chinese herb Curcuma longa. The caveolin-1 (CAV-1) is widely expressed in lung cells and plays a key role in platelet-derived growth factor (PDGF) signaling and cell proliferation. This study aims to investigate the effect of Zed on human bronchial smooth muscle cell (HBSMC) proliferation and explore its potential molecular mechanisms. We assessed the effect of Zed on the proliferation of PDGF-stimulated HBSMCs and performed proteomic analysis to identify potential molecular targets and pathways.
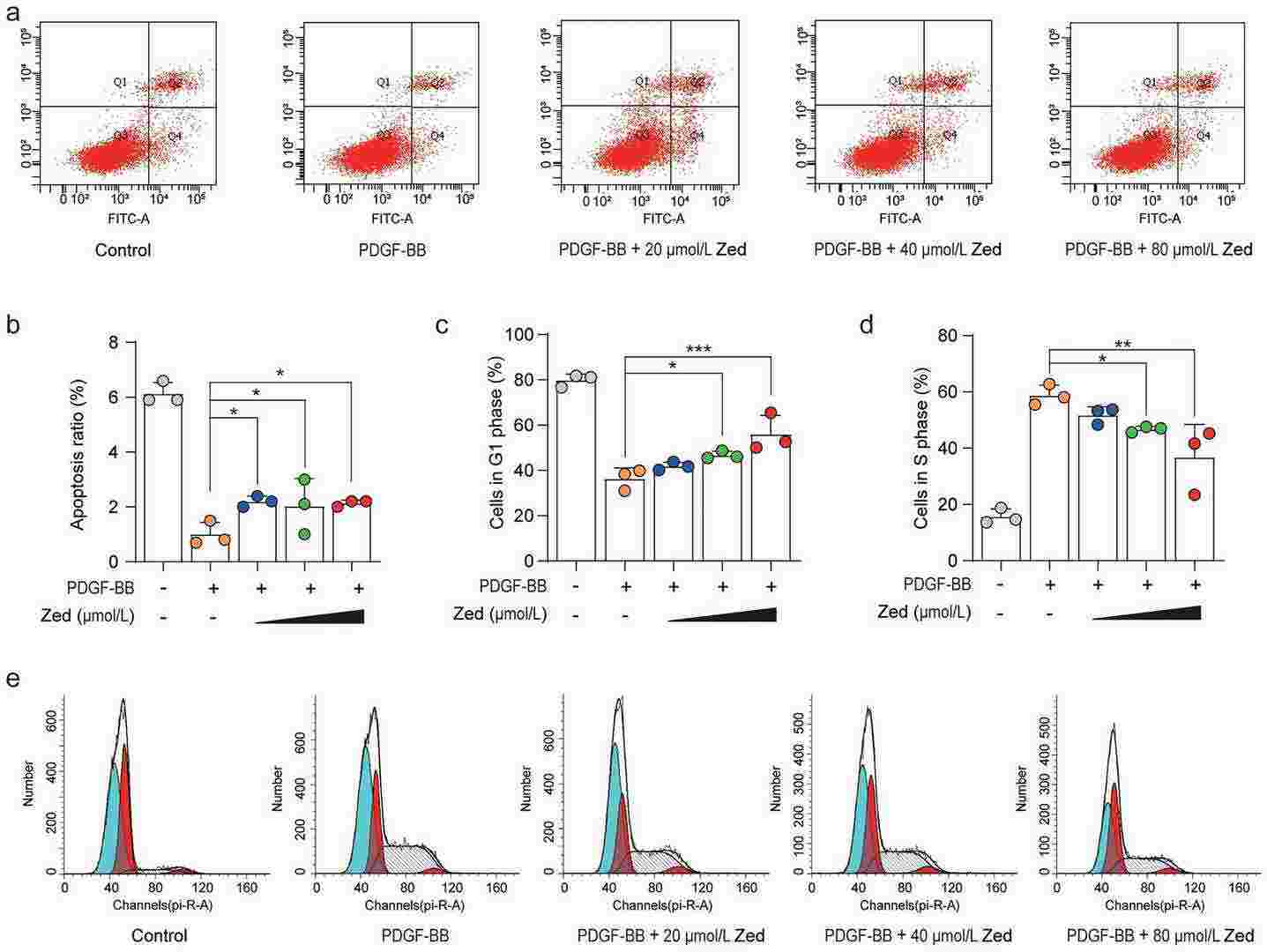 Fig. 1. Zedoarondiol induces cell apoptosis in HBSMCs and blocks proliferation of HBSMCs induced by PDGF-BB in G1 phase (Lyu, Yinglan, et al. 2024).
Fig. 1. Zedoarondiol induces cell apoptosis in HBSMCs and blocks proliferation of HBSMCs induced by PDGF-BB in G1 phase (Lyu, Yinglan, et al. 2024).
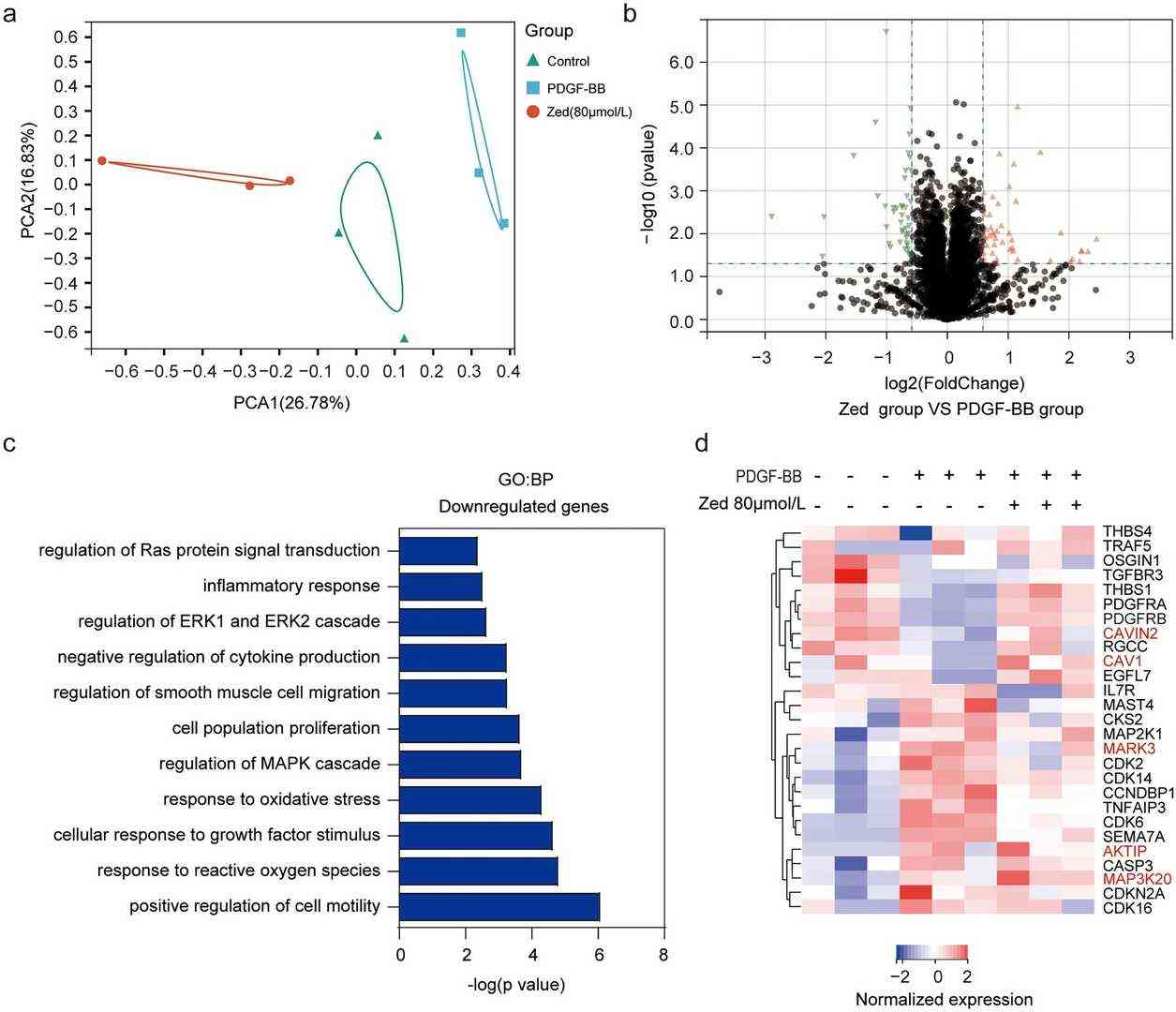 Fig. 2. Quantitative proteomic analysis of the action of Zed on PDGF-BB-induced proliferation in HBSMCs (Lyu, Yinglan, et al. 2024).
Fig. 2. Quantitative proteomic analysis of the action of Zed on PDGF-BB-induced proliferation in HBSMCs (Lyu, Yinglan, et al. 2024).
Nanoplastics Penetrate Human Bronchial Smooth Muscle Cells and Affect Mitochondrial Metabolism
Micro- and nanoplastic particles, including common forms like polyethylene and polystyrene, have been identified as relevant pollutants, potentially causing health problems in living organisms. The mechanisms at the cellular level largely remain to be elucidated. This study aims to visualize nanoplastics in bronchial smooth muscle (BSMC) and small airway epithelial cells (SAEC), and to assess the impact on mitochondrial metabolism.
Healthy and asthmatic human BSMC and SAEC in vitro cultures were stimulated with polystyrene nanoplastics (PS-NPs) of 25 or 50 nm size, for 1 or 24 h. Live cell, label-free imaging by holotomography microscopy and mitochondrial respiration and glycolysis assessment were performed. The 25 and 50 nm NPs were shown to penetrate SAEC, along with healthy and diseased BSMC, and they impaired bioenergetics and induce mitochondrial dysfunction compared to cells not treated with NPs, including changes in oxygen consumption rate and extracellular acidification rate.
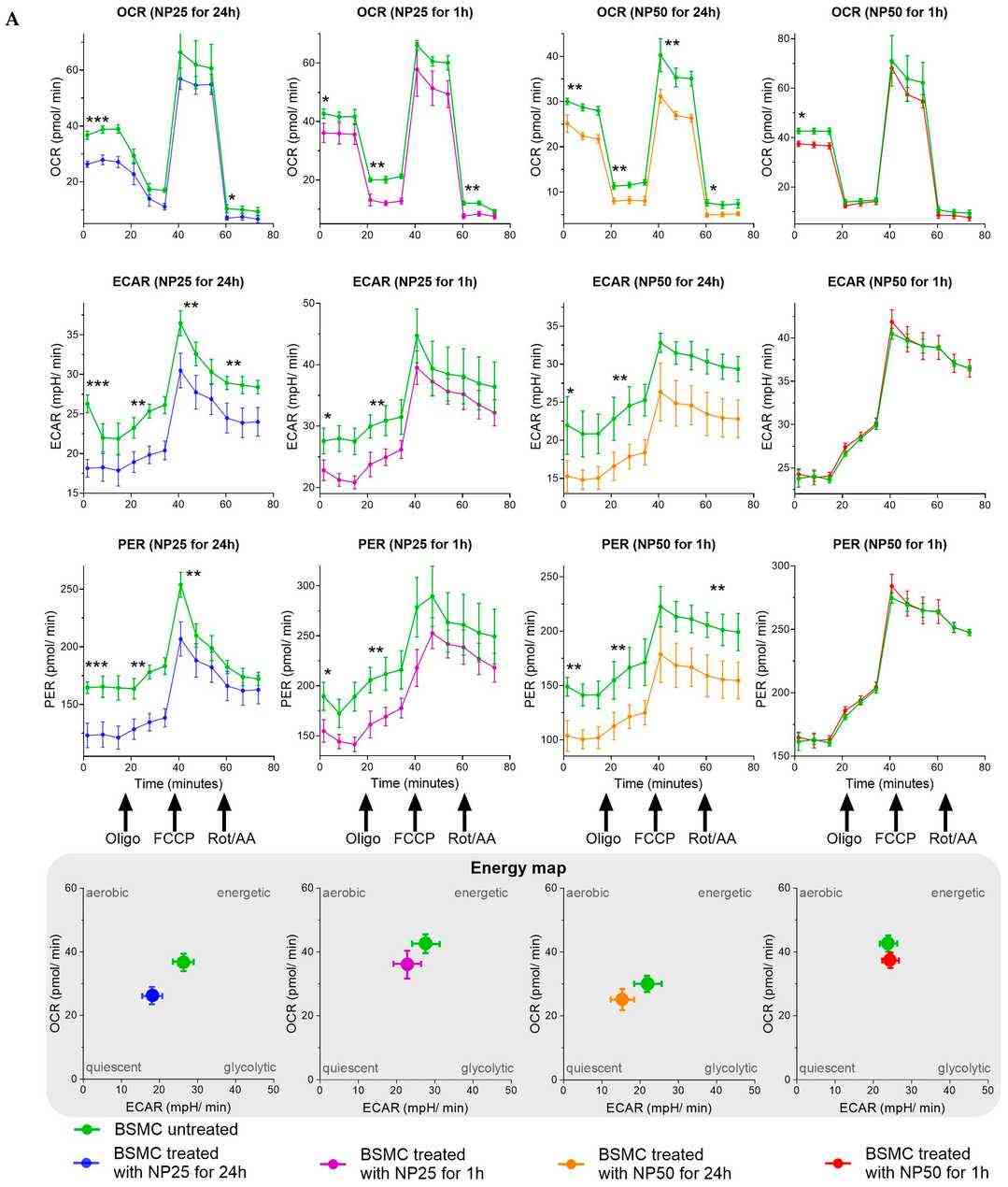
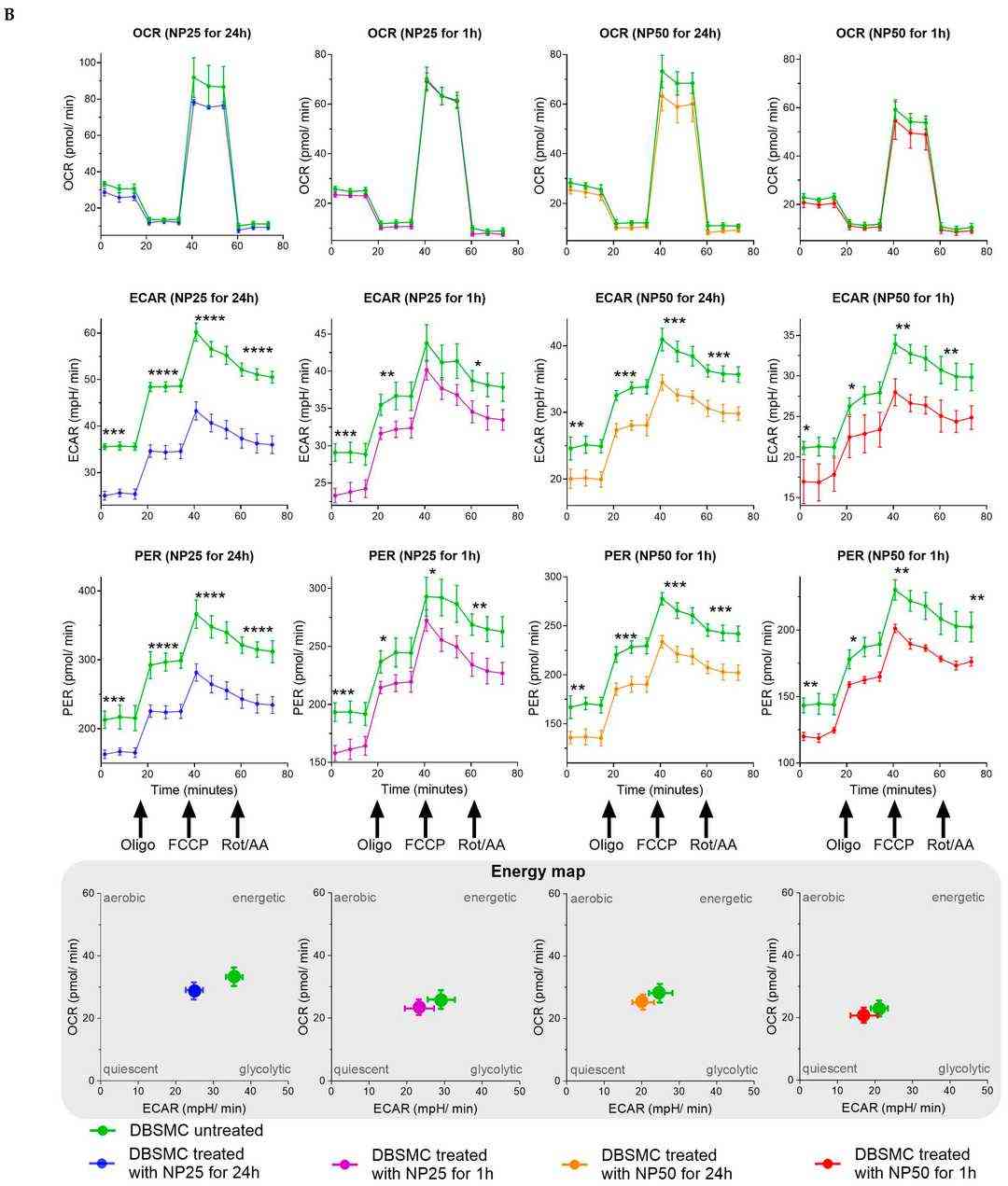 Fig. 3. The impact of polystyrene nanoplastics (PS-NPs) on the mitochondrial metabolism in human healthy bronchial smooth muscle cells (BSMC) and asthmatic (diseased) bronchial smooth muscle cells (DBSMC) (Winiarska, Ewa, et al. 2024).
Fig. 3. The impact of polystyrene nanoplastics (PS-NPs) on the mitochondrial metabolism in human healthy bronchial smooth muscle cells (BSMC) and asthmatic (diseased) bronchial smooth muscle cells (DBSMC) (Winiarska, Ewa, et al. 2024).
The assessment included measurements of oxygen consumption rate (OCR), extracellular acidification rate (ECAR), and total proton efflux rate (PER) under basal conditions, as well as in response to the following mitochondrial inhibitors: oligomycin (Oligo), cyanide-4-(trifluoromethoxy)phenylhydrazone (FCCP), and a combination of rotenone and antimycin A (Rot/AA).
Ask a Question
Write your own review




