
Immortalized Human Endometrial Stromal Cells (HESC)
Cat.No.: CSC-I9213L
Species: Homo sapiens
Source: Endometria
Morphology: Fibroblast-like
Culture Properties: Adherent
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Note: Never can cells be kept at -20 °C.
2) ELISA and RT-PCR were performed to detect IGFBP-1, FN, PRL and PAI-1 secretion and mRNA expression;
3) Western blot and densitometry were conducted to determine the expression of TF and Fas/Fas ligand.
Researchers have created the immortalized human endometrial stromal cells (HESC) cell line using genetic engineering techniques from human endometrial tissues. The endometrial cells serve as fundamental elements which support cyclical changes throughout the menstrual cycle and facilitate embryo implantation during pregnancy. Immortalized HESC cells demonstrate standard features of endometrial stromal cells which show responses to hormonal triggers, especially estrogen and progesterone. For example, immortalized HESC differentiate into secretory-type cells which release essential secretory factors including insulin-like growth factor-1 (IGF-1), tissue factor (TF), and plasminogen activator inhibitor-1 (PAI-1) when exposed to both estrogen and progesterone. The process of endometrial decidualization depends heavily on these factors which create a critical environment for embryo implantation.
Immortalized HESC serve as a research tool to study the periodic alterations of the endometrium while examining hormone reactions and disease pathology. Researchers use hormonal stimuli simulations throughout the menstrual cycle to study both cell differentiation and secretory functions. Immortalized HESC serve as a research tool to explore how endometriosis begins. Research shows that these cells display similar gene expression and secretory profiles to primary endometrial cells when exposed to particular conditions. Furthermore, these cells serve as essential instruments for endometrial regeneration and repair because of their outstanding ability to proliferate and differentiate.
 Fig. 1. Morphological of telomerase-immortalised endometrial stromal cell line THESC (Saleh L, Otti G R, et al., 2011).
Fig. 1. Morphological of telomerase-immortalised endometrial stromal cell line THESC (Saleh L, Otti G R, et al., 2011).
Inhibitory Effects of Estetrol on the Invasion and Migration of Immortalized Human Endometrial Stromal Cells
Endometriosis, affecting 10% of premenopausal and up to 50% of infertile women, involves ectopic growth of endometrial tissue causing pain and infertility. 17β estradiol (E2) enhances lesion growth by activating estrogen receptors, while estetrol (E4), a natural estrogen, might counteract these effects due to its distinct receptor binding properties.
Utilizing immortalized HESCs, the effects of E4 versus E2 on cellular invasion and migration were measured using Matrigel chamber, wound healing, and cell tracking assays. Initially, Wakaktsuki et al. examined how E2 and E4 affect HESC proliferation, finding no impact from either hormone, possibly due to prior viral activation saturating cell growth. Next, they assessed the impact on HESC invasion: E2 at 10–9 M (0.3 ng/mL) increased invasion over 16 and 24 hours (Fig. 1A), while E4 at varied concentrations inhibited it within 16 hours (Fig. 1B), even without E2 (Fig. 1C). For HESC migration, wound healing and cell tracking showed E2 enhanced migration at 10–9 M (0.3 ng/mL) over 8 hours (Fig. 2A), and up to 24 hours, inhibited by E4 (Fig. 2B). Both methods confirmed E2 significantly boosted migration, while E4 markedly inhibited this effect.
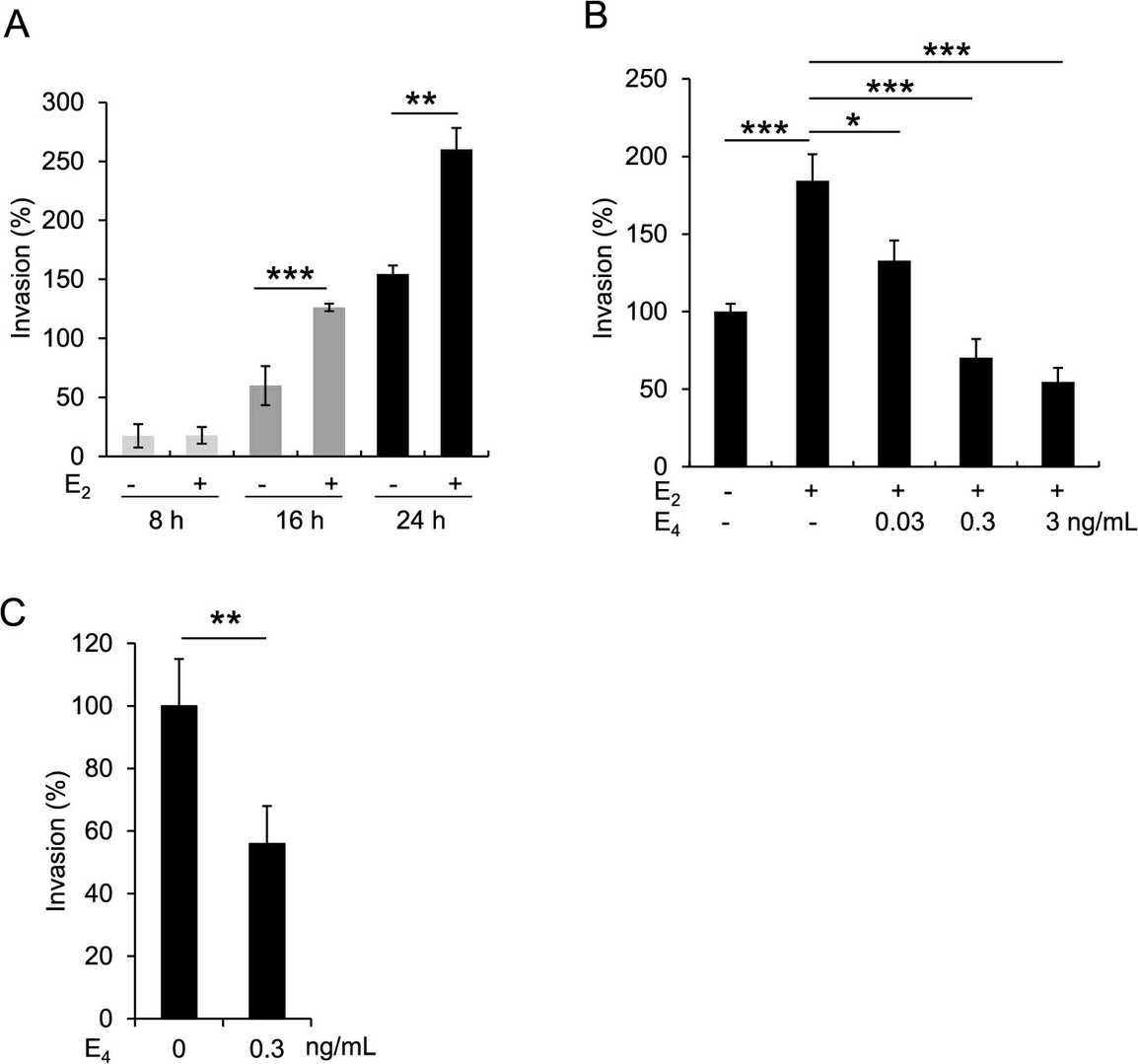 Fig. 1. Activation and inhibition of HESC invasion by E2 and E4, respectively (Wakatsuki A, Lin Y, et al., 2024).
Fig. 1. Activation and inhibition of HESC invasion by E2 and E4, respectively (Wakatsuki A, Lin Y, et al., 2024).
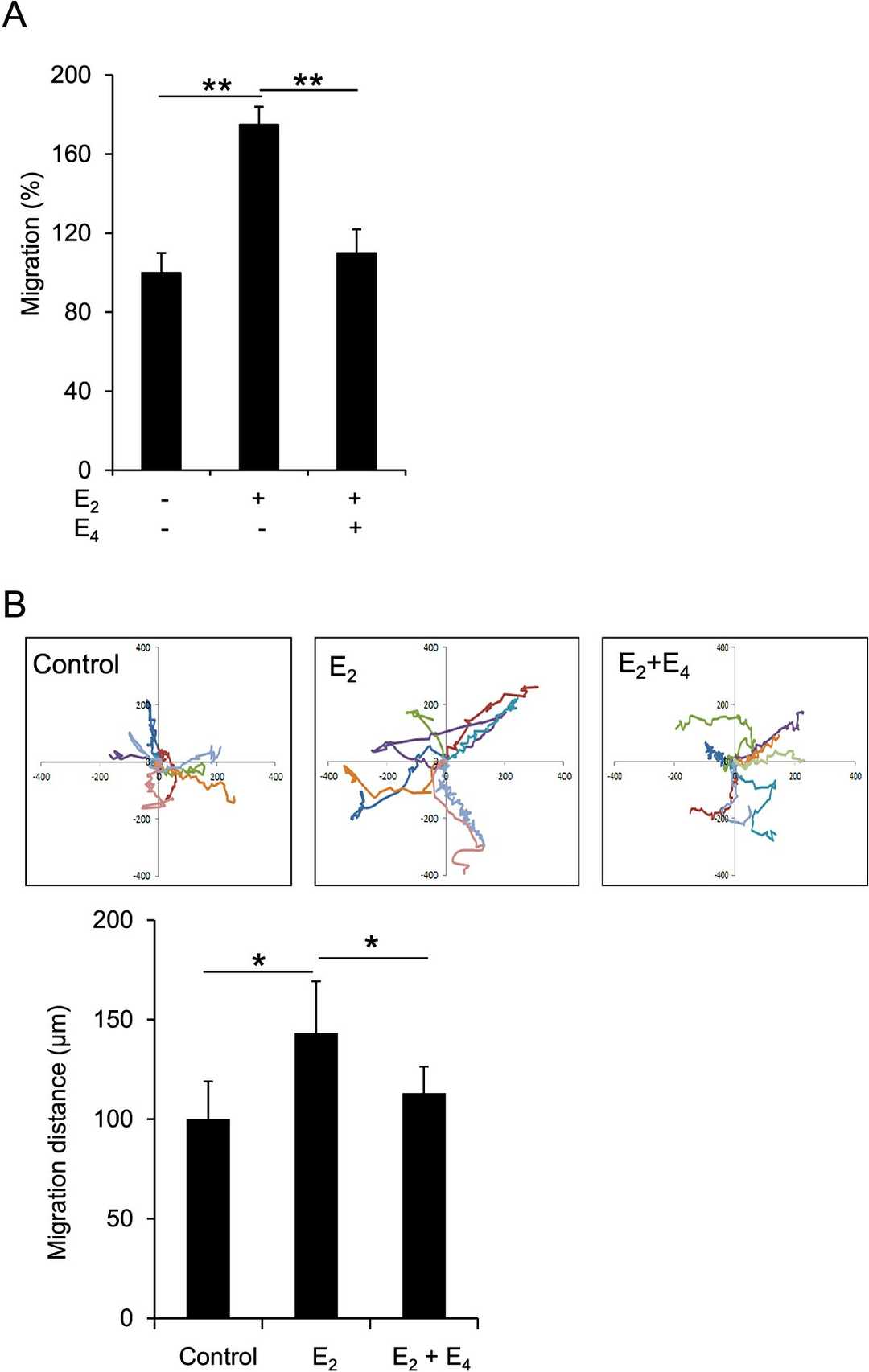 Fig. 2. Inhibition of migration by E4 in HESCs (Wakatsuki A, Lin Y, et al., 2024).
Fig. 2. Inhibition of migration by E4 in HESCs (Wakatsuki A, Lin Y, et al., 2024).
Knockdown of CD44v3 Suppressed the Proliferation and Decidualization of T-HESCs
RIF occurs in 10% of IVF cycles and is linked to poor endometrial receptivity, partly due to inadequate decidualization. CD44 is implicated in cellular functions crucial for implantation. Zhou's investigated the effects of CD44 isoforms, especially CD44v3, on endometrial receptivity in RIF patients, evaluating its influence on proliferation and decidualization of endometrial stromal cells.
They found the expression of CD44v3 was significantly higher in the mid-secretory phase of endometrial stromal cells than in the proliferation phase, but was notably lower in RIF patients. Then, the effects of knockdown and overexpression of CD44v3 in T-HESCs (human telomerase reverse transcriptase-immortalized human endometrial stromal cells) were examined using western blot analysis (Fig. 3A–D, p < 0.01). CD44v3 alterations did not impact T-HESC migration (Fig. 3E–F), but knockdown reduced and overexpression increased cell proliferation (Fig. 3G, p < 0.05). To examine CD44v3's role in decidualization, T-HESCs were treated with E2, P4, and 8-bromo-cAMP. Results showed reduced mRNA levels of PRL and IGFBP1 with CD44v3 knockdown and increased IGFBP1 with overexpression (Fig. 3H, p < 0.05).
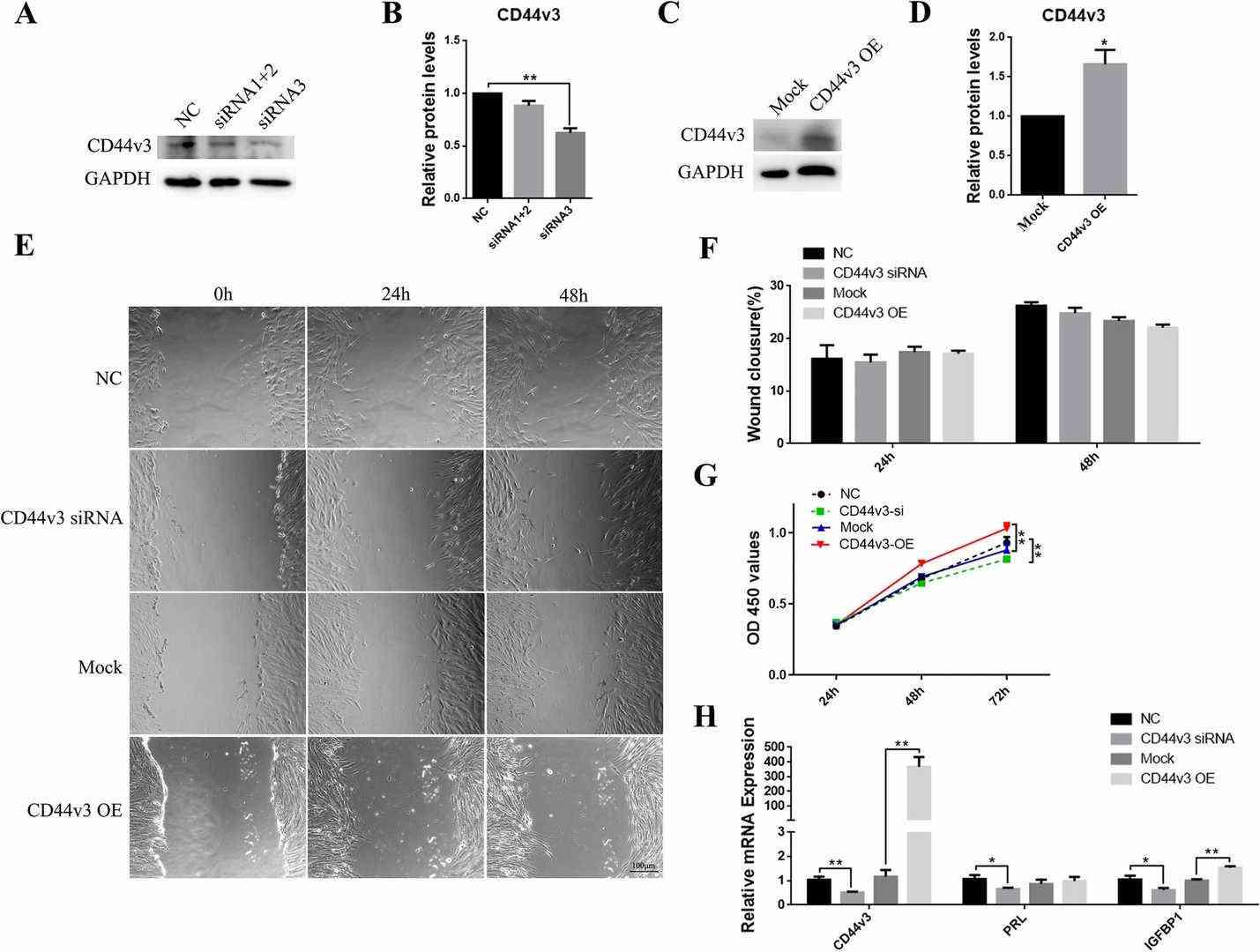 Fig. 3. Changes in cell proliferation and stromal cell decidualization following CD44v3 knockdown/overexpression in T-HESCs (A, C) Western blot and (B, D) densitometric quantification of CD44v3 after the knockdown/overexpression of CD44v3 in T-HESCs (Zhou X, Cao Y, et al., 2022).
Fig. 3. Changes in cell proliferation and stromal cell decidualization following CD44v3 knockdown/overexpression in T-HESCs (A, C) Western blot and (B, D) densitometric quantification of CD44v3 after the knockdown/overexpression of CD44v3 in T-HESCs (Zhou X, Cao Y, et al., 2022).
Ask a Question
Write your own review
- Adipose Tissue-Derived Stem Cells
- Human Neurons
- Mouse Probe
- Whole Chromosome Painting Probes
- Hepatic Cells
- Renal Cells
- In Vitro ADME Kits
- Tissue Microarray
- Tissue Blocks
- Tissue Sections
- FFPE Cell Pellet
- Probe
- Centromere Probes
- Telomere Probes
- Satellite Enumeration Probes
- Subtelomere Specific Probes
- Bacterial Probes
- ISH/FISH Probes
- Exosome Isolation Kit
- Human Adult Stem Cells
- Mouse Stem Cells
- iPSCs
- Mouse Embryonic Stem Cells
- iPSC Differentiation Kits
- Mesenchymal Stem Cells
- Immortalized Human Cells
- Immortalized Murine Cells
- Cell Immortalization Kit
- Adipose Cells
- Cardiac Cells
- Dermal Cells
- Epidermal Cells
- Peripheral Blood Mononuclear Cells
- Umbilical Cord Cells
- Monkey Primary Cells
- Mouse Primary Cells
- Breast Tumor Cells
- Colorectal Tumor Cells
- Esophageal Tumor Cells
- Lung Tumor Cells
- Leukemia/Lymphoma/Myeloma Cells
- Ovarian Tumor Cells
- Pancreatic Tumor Cells
- Mouse Tumor Cells

