Overview of Autoinflammatory Disease Cellular Models
Clinical and Translational Immunology. 2024 Jan 11;13 (1): e1481.
Authors: Şen B, Balcı-Peynircioğlu B.
INTRODUCTION
Systemic autoinflammatory diseases are a heterogeneous group of rare genetic disorders caused by dysregulation of the innate immune system. Understanding the complex mechanisms underlying these conditions is critical for developing effective treatments. Cellular models are essential for identifying new conditions and studying their pathogenesis. Traditionally, these studies have used primary cells and cell lines of disease-relevant cell types, although newer induced pluripotent stem cell (iPSC)-based models might have unique advantages.
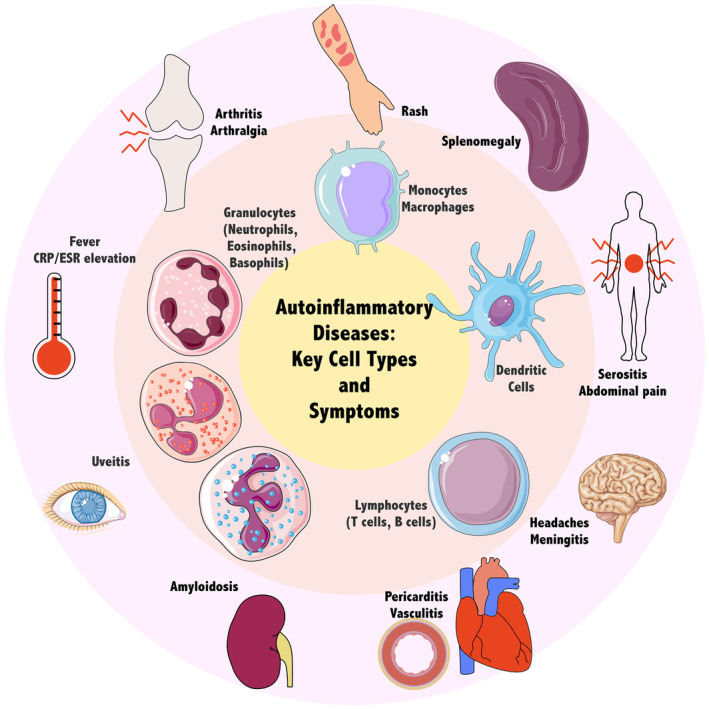 Fig. 1 Hallmarks of autoinflammation and major effector cell types.
Fig. 1 Hallmarks of autoinflammation and major effector cell types.
Human Primary Cells
Cells isolated from patient samples and cultured in vitro are an essential resource for studying disease. Primary cells provide a more physiologically relevant model than cell lines. Thus, these models are especially useful when dealing with previously undefined or rare diseases for which other models have not been established. However, human primary cells have a limited lifespan in cell culture conditions.
- As blood is an easily accessible source of primary cells, peripheral blood mononuclear cells (PBMCs) are the cells of choice when investigating immune diseases, including SAIDs. PBMCs consist of a diverse population of immune cells, including lymphocytes, monocytes, dendritic cells, and natural killer cells, so they are widely used in autoinflammatory disease research as they represent the general state of the immune system.
- Neutrophils, another major player in innate immunity, can also be obtained from patients' blood; however, they are more challenging to isolate, are viable for a shorter period than PBMCs, and are prone to activation and apoptosis under culture conditions. These properties necessitate researchers to work quickly with neutrophils, making them a less attractive choice for modeling.
- Fibroblasts derived from skin biopsies of patients have also been used to investigate autoinflammatory diseases. Although relatively invasive to acquire, primary fibroblast cultures are easier to set up and maintain compared to other cell types, such as immune cells.
Cell Lines
Immortalized cell lines are ubiquitous models for monocytes/macrophages used in studies of innate immune mechanisms, host-pathogen interactions, and roles in disease. Compared to primary cells, cell lines are easier to handle and have a homogeneous genetic background. However, these cells usually have malignant heritage and genetic changes because of adaptation to culture conditions, making them of uncertain biological relevance. Another prevalent problem is cross-contamination with other cell lines.
One widely used cell line in SAIDs research is THP-1, a monocyte-like cell line isolated from an acute myeloid leukemia patient. This line is morphologically and functionally similar to monocytes and can be differentiated in vitro into macrophage-like cells. U-937 is another monocytic cell line, isolated from a patient with histiocytic lymphoma, that is also used widely in autoinflammatory disease research. These cells display a similar phenotype to THP-1 cells, can be cultured in similar conditions, and can also be differentiated into macrophage-like cells.
Patient-Derived iPS Cells
The discovery of induced pluripotent stem cells (iPSCs), somatic cells that have been reprogrammed into an embryonic stem cell-like state, has opened new avenues of research in disease modeling, regenerative medicine, and drug discovery. One and a half decades after their discovery, the introduction of various cell types as a source for iPSCs (e.g. fibroblasts, blood cells, urinary epithelial cells), the discovery of non-integrative reprogramming methods (e.g. Sendai virus, episomal, mRNA transfection), and new developments that significantly increased reprogramming efficiency have expanded the accessibility of the platform. iPSCs derived from patient samples provide an inexhaustible resource of disease-specific cells, making them an attractive choice for disease modeling.
To be useful in modeling autoinflammatory disorders, iPSCs need to be differentiated into the relevant cell types; indeed, many different protocols for the differentiation of iPSCs towards monocytes/macrophages have been developed, with varying techniques and efficiencies. These differentiation protocols generally last 3-4 weeks and rely on sequential incubation with various combinations of cytokines and growth factors that mimic primitive hematopoiesis. iPSC-derived macrophages (iPSDMs) have been studied more extensively than monocytes, and their morphological and functional phenotypes have been compared with those of primary monocyte-derived macrophages (MDMs).
Creative Bioarray Relevant Recommendations
| Service/Product Types | Description |
| Primary Cells | The team of cell culture experts at Creative Bioarray provides you with a large and unique collection of high-purity, low-passage human and animal primary cells. |
| Immortalized Cell Lines | Creative Bioarray has developed the most comprehensive immortalized cell lines comprising human-immortalized cells, mouse-immortalized cells, and other immortalized cells. |
| Stem Cell Research | Whether you want to obtain and expand pluripotent cells, differentiate them along specific lineages, or edit your cells, our products and services support your goals. |
| Inflammation and Autoimmune Disease Models | Our inflammatory and autoimmune disease models can serve as the assay basis for the analysis of biomarkers and provide accurate experimental capabilities to elucidate the role of candidate compounds in the treatment of each disease. |
RELATED PRODUCTS & SERVICES
Reference
- Şen B, Balcı-Peynircioğlu B. (2024). "Cellular models in autoinflammatory disease research." Clin Transl Immunology. 13 (1), e1481.