
Human Amniotic Epithelial Cells (HAmEpiC)
Cat.No.: CSC-7842W
Species: Human
Source: Placenta
Cell Type: Epithelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
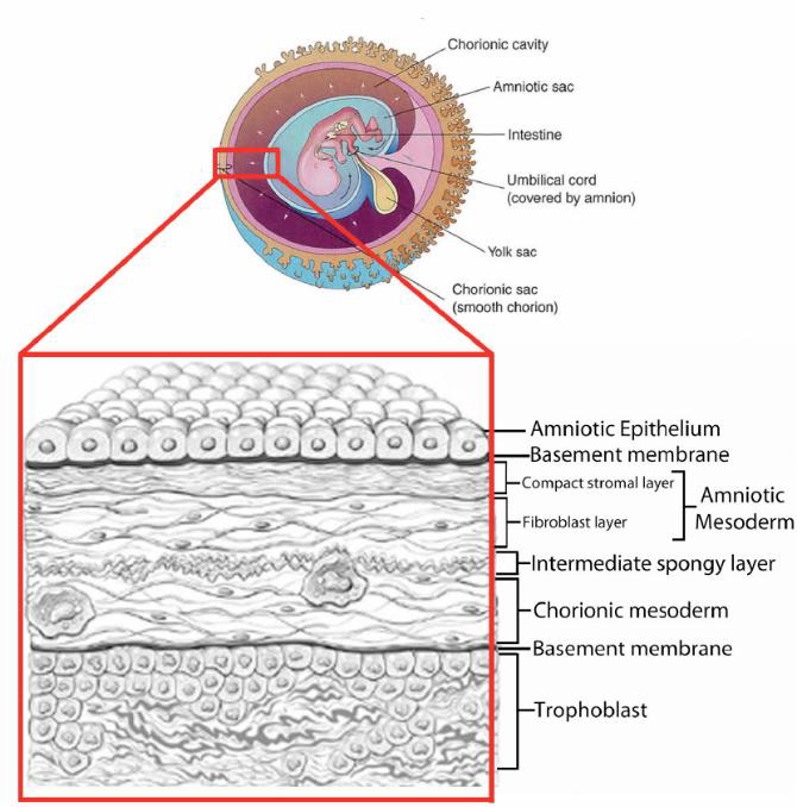
Human amniotic epithelial cells (hAECs) are a unique population of fetal‑derived cells isolated from the innermost layer of the term placenta-the amniotic membrane-where a single‑cell epithelial sheet rests on a basement membrane that directly contacts amniotic fluid. hAECs are derived from the pre‑gastrulation epiblast and maintain epigenetic memory of embryonic ectoderm, while expressing pluripotency markers (OCT‑4, NANOG and SOX‑2), epithelial markers (E‑cadherin, cytokeratins) and a subset of mesenchymal markers (CD29, CD90, CD105) due to partial epithelial‑mesenchymal transition during in vitro culture. Morphologically, hAECs appear as cuboidal to columnar cells with microvilli on their apical surface; they adhere rapidly to culture substrates, reach confluence within 3-4 days, and display limited proliferative capacity (≈ 2-3 passages) before senescence or EMT‑driven changes occur.
Functionally, hAECs secrete a broad range of growth factors (HGF, bFGF, TGF‑β), neurotrophic factors and anti‑inflammatory cytokines (IL‑10, PGE2), while expressing low levels of MHC‑I and little to no MHC‑II, which confers immune‑privilege and the ability to suppress mixed‑lymphocyte reactions. These properties underpin a broad spectrum of pre‑clinical applications: tissue‑engineered membranes for wound healing, corneal surface reconstruction, and skin grafts; differentiation into hepatocyte‑like, pancreatic‑β, cardiomyocyte‑like, and neural cells for organ‑specific regeneration; and immunomodulation in graft‑versus‑host disease, autoimmune disorders, and neurodegenerative models such as Parkinson's and Alzheimer's disease. Importantly, hAECs are non‑tumorigenic in vivo and can be harvested without ethical controversy, making them a promising allogeneic cell‑therapy platform for regenerative medicine.
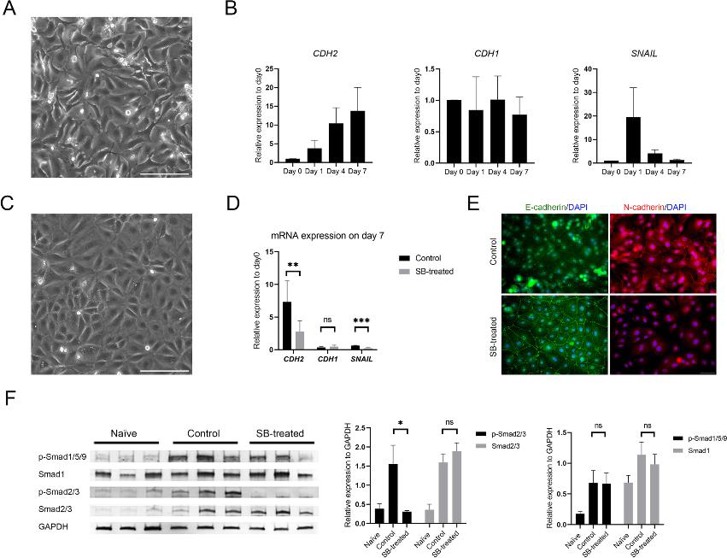
hAECs Underwent TGF-β-dependent EMT Shortly after Starting Cell Culture
Human amniotic epithelial cells (hAECs) are pluripotent placental stem cells with the potential to differentiate into all three germ layers. They exhibit TGF-β-dependent epithelial-mesenchymal transition (EMT), yet the role of EMT in hAECs for stemness or differentiation is currently unknown. Takano et al. studied how TGF-β-dependent EMT regulates the stemness of hAECs.
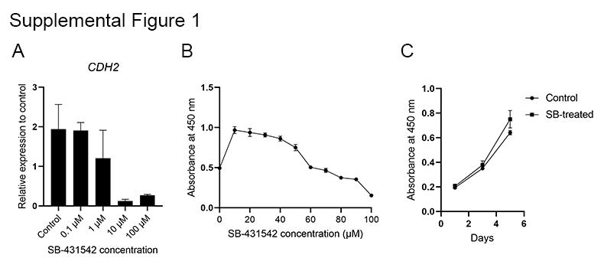
Cells acquired fibroblast-like morphology within 7 days of cultivation (Fig. 1A). The mRNA expression of the mesenchymal marker CDH2 was upregulated, whereas the epithelial marker CDH1 was not downregulated (Fig. 1B). The EMT marker SNAIL was transiently upregulated one day after culture initiation. To confirm TGF-β dependency of hAEC EMT, the selective ALK5 inhibitor SB-431542 was added to the culture media. Through dose-dependent RT-qPCR and cell viability assays researchers optimized the compound concentration to 10 µM. This suppressed CDH2 mRNA expression on day 7 (Fig. 2A) without reducing cell viability (Fig. 2B). The TGF-β signaling inhibition by 10 µM SB-431542 maintained the typical cobblestone-like epithelial morphology (Fig. 1C). Cell viability (99.9±0.13%) and growth did not differ between SB-treated and control cells (Fig. 2C). On day 7, SB-treated cells exhibited suppressed CDH2 and SNAIL mRNA expression, while CDH1 expression was unchanged (Fig. 1D). Immunocytochemistry showed N-cadherin at cell junctions in control cells and E-cadherin in SB-treated cells (Fig. 1E).
Ask a Question
Write your own review
