
Rat Brain Microvascular Endothelial Cells
Cat.No.: CSC-C1972
Species: Rat
Source: Brain
Cell Type: Endothelial Cell; Microvascular Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
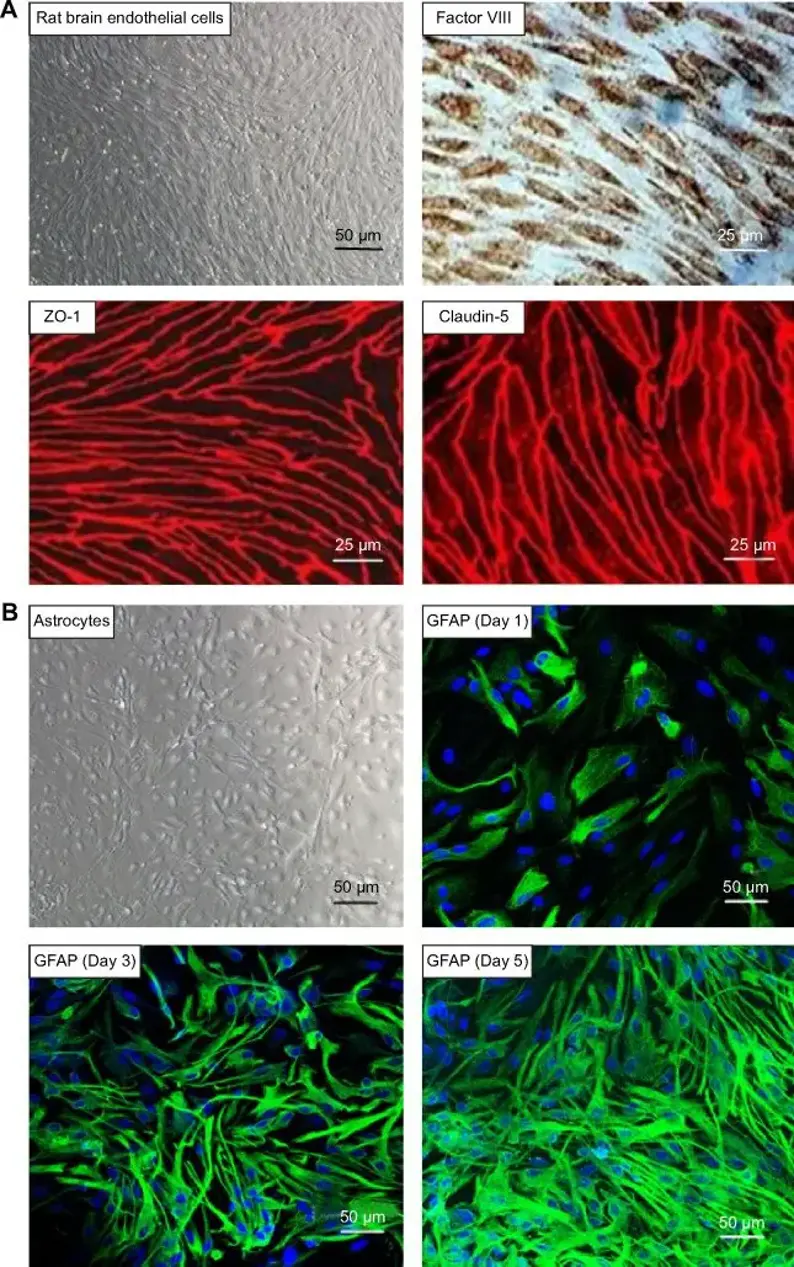
Rat Brain Microvascular Endothelial Cells (RBMVECs) are endothelial cells which comprise the structural and functional element of the BBB. They differ from endothelial cells of the periphery by possessing unique morphological and physiological characteristics. These cells have specialized tight junctions (zonula occludens and claudins), high electrical resistance and low rates of pinocytosis. As such, these cells tightly regulate movement of ions and nutrients, as well as cells into the central nervous system from blood circulation. Regulation of materials into CNS tissue by RBMVECs contributes to neural homeostasis and protects tissues from harmful toxins and pathogens.
Due to their important function in barrier maintenance and nutrient transport into the CNS tissue, RBMVECs are widely used as an in vitro model for studying neurovascular coupling, drug delivery to the brain, and cerebrovascular disease pathogenesis. RBMVECs are often used to understand how barrier permeability may be disrupted by inflammatory mediators or reactive oxygen species in disease models such as stroke, Alzheimer's disease, and multiple sclerosis. Additionally, these cells express transporters which drug developers commonly screen CNS drug candidates for including P-glycoprotein and GLUT-1. RBMVECs can be obtained as either primary cells or immortalized cells.
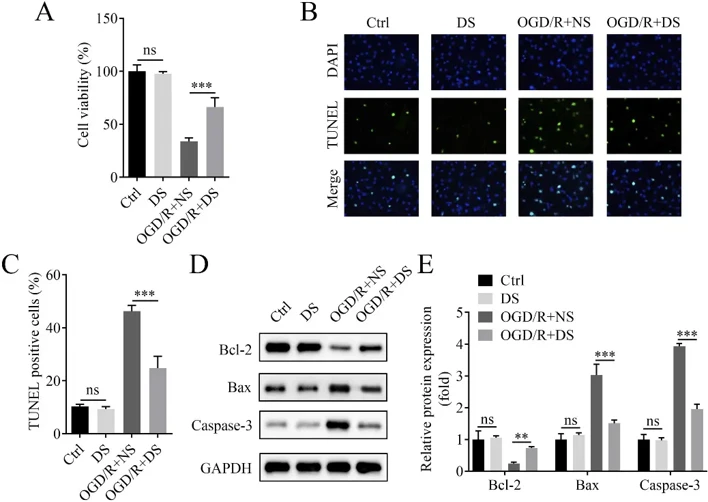
DS Increased Viability and Suppressed Apoptosis of OGD/R-treated RBMVECs
Buyang Huanwu Decoction (BHD) is commonly applied in clinic for ischemic cerebral vascular diseases in China. Song's team aimed to study the effect of BHD on ischemic stroke (IS) in middle cerebral artery occlusion (MCAO) rats and oxygen-glucose deprivation/reoxygenation (OGD/R) in rat brain microvascular endothelial cells (RBMVECs). They found that BHD significantly alleviated infarction volume, neurological function deficit and BBB permeability in MCAO rats. Normal saline (NS) or BHD-derived serum (DS) was applied to treat normal and OGD/R RBMVECs in vitro. Compared to NS, DS treatment significantly increased cell viability (Fig. 1A) and decreased cell apoptosis in OGD/R-treated RBMVECs as indicated by fewer TUNEL-positive cells (Fig. 1B-C). DS treatment also upregulated Bcl-2 and downregulated Bax and Caspase-3 protein expression in OGD/R-treated RBMVECs compared to NS treatment (Fig. 1D-E). Taken together, BHD-derived DS increases viability and inhibits apoptosis in OGD/R-treated RBMVECs.
Ask a Question
Write your own review





