
Lu65
Cat.No.: CSC-C4620J
Species: Homo sapiens (Human)
Source: Lung
Morphology: Epithelial-like
Culture Properties: Adherent, many floating cells are observed
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Shipping Condition: Dry Ice.
Lu65 (also known as Lu-65 or L-65) is a human cancer cell line derived from the tumor tissue of a patient with lung giant cell carcinoma, an extremely aggressive variant of NSCLC. In terms of histopathology, Lu65 is a rare subtype of lung cancer that is considered high-grade pleomorphic. Lu65 cells are known to have a homozygous TP53 mutation and an activating KRAS mutation (most commonly G12C).
Physiologically, Lu65 cells show an adherent growth pattern with a large pleomorphic and often multinucleated phenotype that is consistent with their classification as a "giant cell" lung cancer. A major biological feature of the Lu65 cell line is its genetic mutations, including a homozygous TP53 mutation and an activating KRAS mutation, which are associated with a high rate of proliferation and resistance to apoptosis.
In the scientific literature, Lu65 has been used as a cell line in xenograft experiments for many studies since it can form rapidly growing and poorly differentiated tumors in immunocompromised mice that typically recapitulate the original large-cell morphology. Therefore, the cell line is commonly used as a model to assess the efficacy of new targeted cancer therapeutics, especially KRAS inhibitors, as well as EMT and invasion.
Direct Tumor Recognition by and Cytokine Expression Status of PLAC1-Specific CD4 Helper T Cells
KRAS is a frequently mutated oncogene in cancers, including non-small cell lung cancer (NSCLC). While KRAS G12C inhibitors like AMG510 have shown promise in early clinical trials, resistance mechanisms remain unclear. Adachi et al. aimed to identify intrinsic and acquired resistance mechanisms to KRAS G12C inhibitors using a panel of KRAS G12C-mutant lung cancer cell lines.
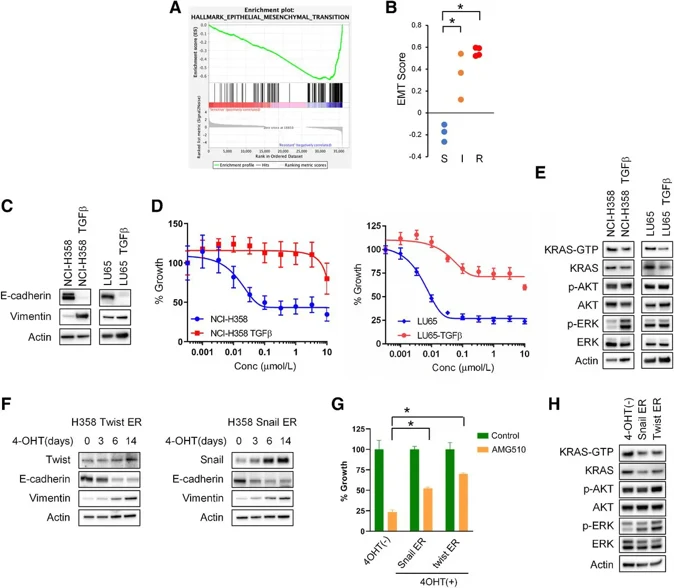
In addition to a KRAS-dependency signature associated with sensitivity to AMG510, GSEA revealed a significant enrichment of genes related to epithelial-mesenchymal transition (EMT) in AMG510-resistant cell lines (Fig. 1A). Sensitivity to AMG510 was strongly correlated with EMT scoring derived from various cancer-specific transcriptomic EMT signatures (Fig. 1B). To investigate whether EMT contributes to resistance to the KRAS G12C inhibitor AMG510, they induced EMT through chronic TGFβ treatment in the epithelial marker-positive and AMG510-sensitive NCI-H358 and LU65 cells. Remarkably, inducing EMT in these cells was sufficient to confer resistance to AMG510 (Fig. 1C and D). EMT induction led to changes in the expression of several receptor tyrosine kinases (RTKs), such as ERBB3 and FGFR1, and coincided with the suppression of E-cadherin (Fig. 1C). Importantly, EMT induction resulted in reduced expression and activation of KRAS, similar to what was observed in AMG510-insensitive cell lines (Fig. 1E). Notably, despite the suppression of KRAS, ERK phosphorylation was paradoxically higher in EMT-induced cells.
Ask a Question
Write your own review
- Adipose Tissue-Derived Stem Cells
- Human Neurons
- Mouse Probe
- Whole Chromosome Painting Probes
- Hepatic Cells
- Renal Cells
- In Vitro ADME Kits
- Tissue Microarray
- Tissue Blocks
- Tissue Sections
- FFPE Cell Pellet
- Probe
- Centromere Probes
- Telomere Probes
- Satellite Enumeration Probes
- Subtelomere Specific Probes
- Bacterial Probes
- ISH/FISH Probes
- Exosome Isolation Kit
- Human Adult Stem Cells
- Mouse Stem Cells
- iPSCs
- Mouse Embryonic Stem Cells
- iPSC Differentiation Kits
- Mesenchymal Stem Cells
- Immortalized Human Cells
- Immortalized Murine Cells
- Cell Immortalization Kit
- Adipose Cells
- Cardiac Cells
- Dermal Cells
- Epidermal Cells
- Peripheral Blood Mononuclear Cells
- Umbilical Cord Cells
- Monkey Primary Cells
- Mouse Primary Cells
- Breast Tumor Cells
- Colorectal Tumor Cells
- Esophageal Tumor Cells
- Lung Tumor Cells
- Leukemia/Lymphoma/Myeloma Cells
- Ovarian Tumor Cells
- Pancreatic Tumor Cells
- Mouse Tumor Cells





