
Human Thyroid Epithelial Cells
Cat.No.: CSC-C4879L
Species: Human
Source: Thyroid
Cell Type: Epithelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Never can cryopreserved cells be kept at -20 °C.
Human thyroid epithelial cells primarily originate from thyroid tissue, specifically from the epithelial cells of thyroid follicles. Located in the neck below the thyroid cartilage and in front of the trachea, the thyroid gland is a key endocrine organ composed of numerous follicles. Each follicle consists of a central cavity surrounded by a layer of epithelial cells. Thyroid epithelial cells produce and release the thyroid hormones T3 and T4 into the bloodstream by iodinating tyrosine and regulate gene expression throughout the body, resulting in a wide range of physiological processes, including metabolism, growth and development, and nervous system functions. These cells can also take up iodide ions from the blood and subsequently conjugate them with tyrosine, resulting in thyroid hormone precursors, which are ultimately secreted extracellularly.
Thyroid epithelial cells are often studied with respect to autoimmune diseases, including Graves' disease and Hashimoto's thyroiditis. Abnormal expression of the HLA-DR antigens on the surface of thyroid epithelial cells in Graves' disease may play a role in triggering autoimmune responses. Thyroid epithelial cells are also an important model system for the study of thyroid hormone synthesis, secretion, and regulation. For instance, the CI-huThyrEC cell line is used in screening of endocrine disruptors, in order to test the effect of environmental toxins on thyroid function.
Expression of Collagen XIII in Tissues of the Thyroid and Orbit with Relevance to Thyroid-Associated Ophthalmopathy
Antibodies against collagen XIII have previously been identified in patients with active thyroid-associated ophthalmopathy (TAO). Although collagen XIII expression has been described in extraocular muscles and orbital fat, its detailed localization in extraocular and thyroid tissues and the connection to autoimmunity for collagen XIII remain unclear.
Using immunostaining and RT-qPCR on human and mouse tissues, with Col13a1−/− mice as controls, Norman et al. found collagen XIII in extraocular muscles, orbital blood vessels, and thyroid epithelium. To identify the potential cellular source of COL13A1 upregulation, they treated human thyroid epithelial cells and fibroblasts with TGF-β1 and TNF. Addition of TGF-β1 to the growth medium induced COL13A1 expression in the thyroid epithelial cells after 1d or 2d of treatment (Fig. 1I), but when the same cells were grown in depleted medium the addition of TGF-β1 did not upregulate COL13A1 (Fig. 1J). TNF administration did not affect the expression of COL13A1 (Figs. 1I and J). The positive controls for the treatments were upregulation of TGF-β induced (TGFBI) and intercellular adhesion molecule 1 (ICAM1).30–32 Thyroid fibroblasts did not upregulate COL13A1 in response to either treatment when TGFBI and matrix metalloproteinase 9 (MMP9) were used as positive controls.
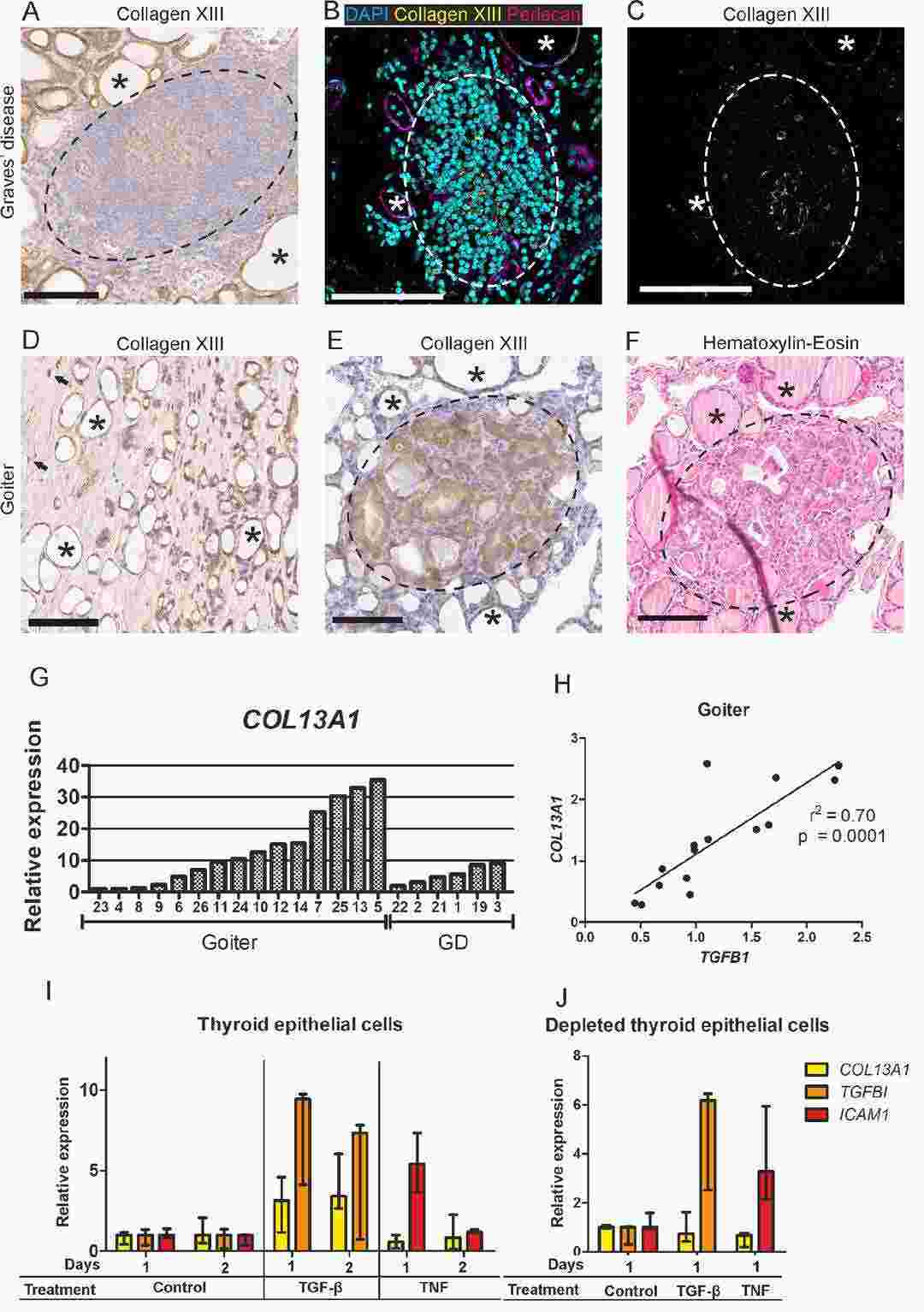 Fig. 1. Collagen XIII in goiter and Graves' disease thyroids (Norman O, Vornanen T, et al., 2024).
Fig. 1. Collagen XIII in goiter and Graves' disease thyroids (Norman O, Vornanen T, et al., 2024).
CTHRC1 was Upregulated in ATC Tissues and Cell Lines
Anaplastic thyroid carcinoma (ATC) is an aggressive cancer with a high mortality rate and limited treatment options. The pathogenesis of ATC is complex and not fully understood. Recent data analysis from GEO and TCGA databases revealed that collagen triple helix repeat containing-1 (CTHRC1) is specifically upregulated in ATC tissues and negatively correlated with overall survival. This study aims to investigate the role of CTHRC1 in ATC progression by examining its effects on tumor cell proliferation, migration, and invasion.
Analysis of CTHRC1 expression in ATC and normal thyroid tissues based on the GEO dataset GSE33630 and GSE65144 showed a significant upregulation of CTHRC1 in ATC tissues (Fig. 2A). Furthermore, CTHRC1 upregulation was found in thyroid cancer (TC) tissues compared to normal tissues using the TCGA database (Figs. 2B and C). Kaplan–Meier plots based on the TCGA database showed the shortening of OS in patients with TC with high CTHRC1 expression (Fig. 2D). Western blotting and quantitative real-time PCR (qRT-PCR) analysis compared CTHRC1 levels in normal human thyroid epithelial cells (Nthy-ori3-1) and ATC cells (THJ-16T, T238, and SW1736). The results showed that ATC cell lines had a markedly higher expression of CTHRC1 (Figs. 2E and F).
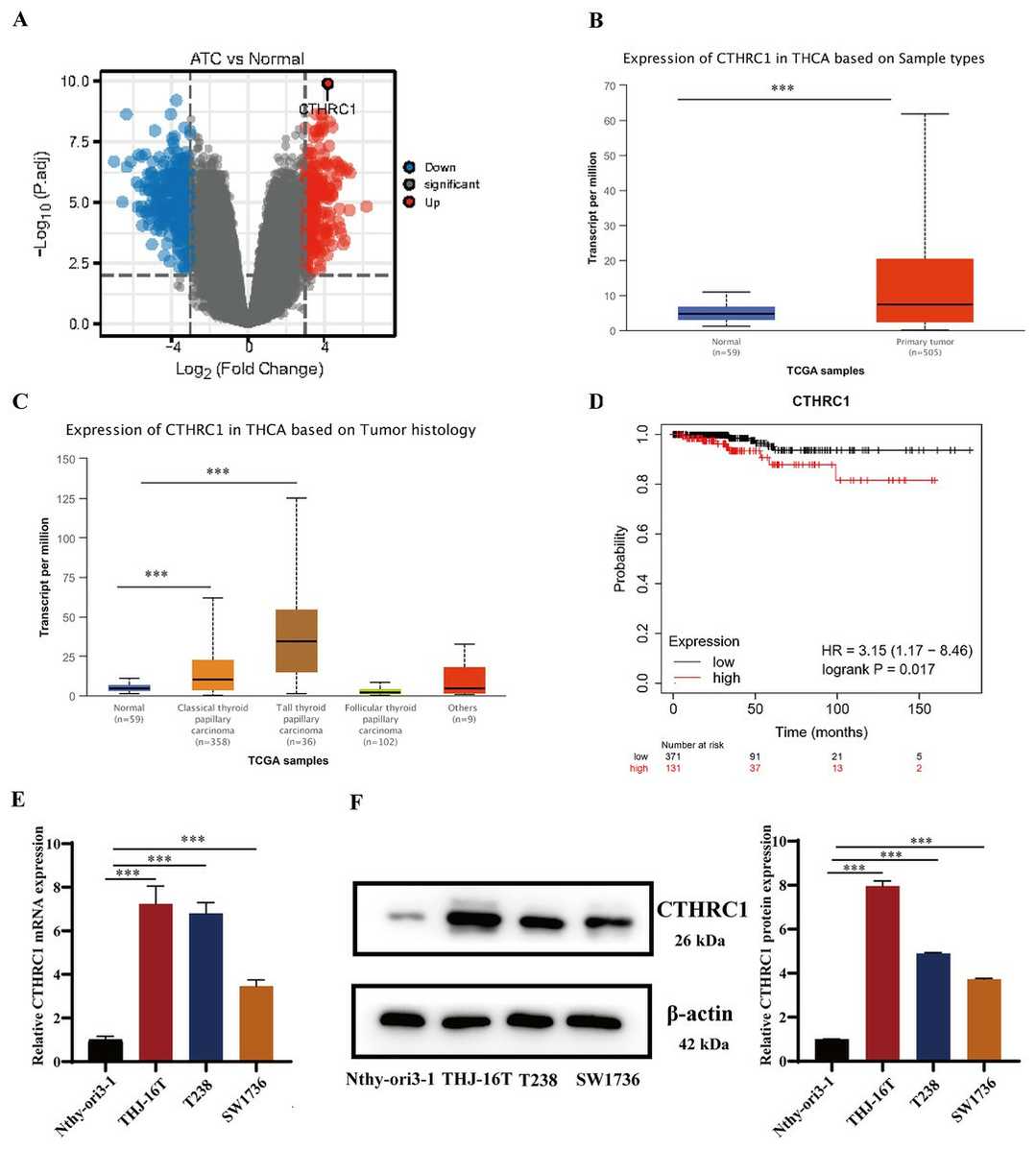 Fig. 2. CTHRC1 was upregulated in ATC tissues and cell lines (Chen Y, Jia L, et al., 2023).
Fig. 2. CTHRC1 was upregulated in ATC tissues and cell lines (Chen Y, Jia L, et al., 2023).
Ask a Question
Write your own review
