
Human Dental Pulp Cells (RA)
Cat.No.: CSC-C3598
Species: Human
Source: Dental Pulp; Tooth
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Rheumatoid arthritis is a chronic, systemic inflammatory disorder that may affect many tissues and organs but principally attacks the joints, producing an inflammatory synovitis that often progresses to destruction of the articular cartilage and ankylosis of the joints.
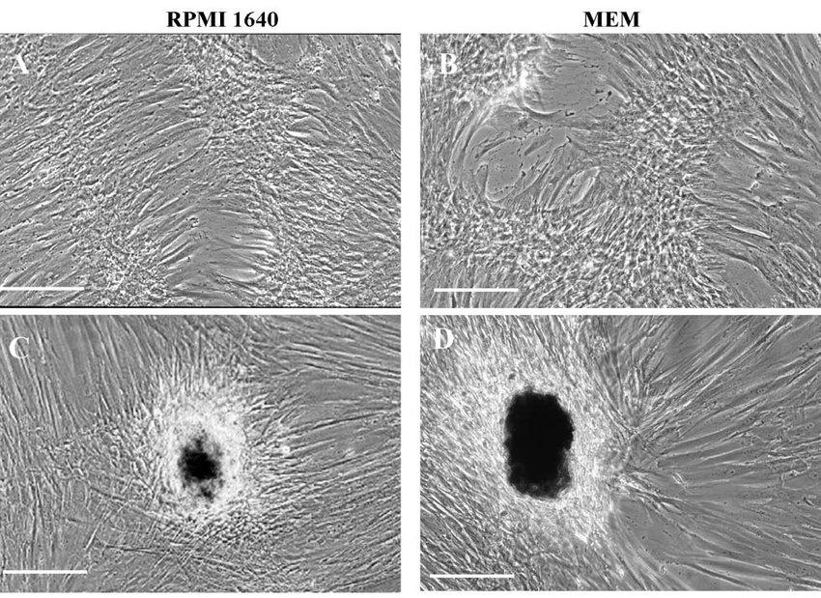
Human dental pulp stem cells (DPSCs) are a population of multipotent dental pulp stem cells that are considered a promising source of pluripotent adult stem cells. They are characterized by their self-renewal, multilineage differentiation ability, as well as odontoblastic, adipocytic, osteoblastic and neural differentiation potential. DPSCs are isolated from the dental pulp, the soft connective tissue within the pulp chamber of the tooth, which is surrounded by several layers of hard tissues including enamel and dentin. They are cultured in vitro as a population of fibroblast-like cells with high proliferative and clonal-forming ability. DPSCs have been investigated and utilized extensively in regenerative dentistry, tissue engineering and regenerative medicine for dental tissue regeneration, bone tissue engineering and neural tissue engineering. They have also been found to have immunomodulatory properties.
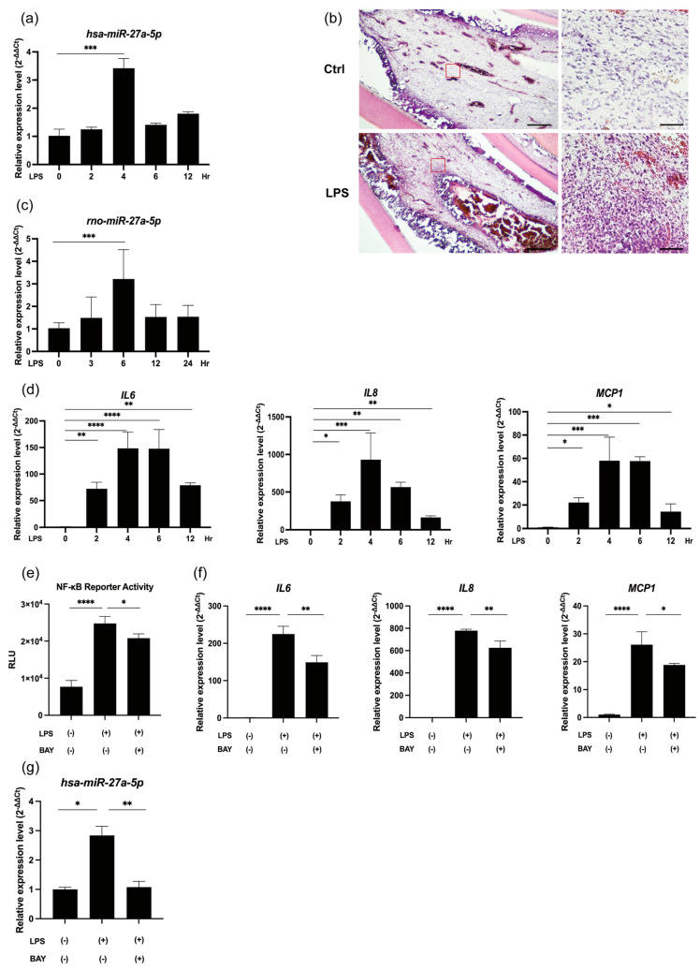
LPS/NF-κB Signaling Promotes miR-27a-5p Expression and Proinflammatory Mediator Levels in LPS-Stimulated hDPCs
MicroRNA-27a-5p (miR-27a-5p) was significantly upregulated in dental pulp inflammation, yet its underlying mechanisms remain unclear. Wang's team used LPS-stimulated human dental pulp cells (hDPCs) and rat incisor pulp tissue explants, transfected with miR-27a-5p mimics and inhibitors, to investigate how miR-27a-5p affects the expression of proinflammatory cytokines and NF-κB signaling pathways.
LPS application significantly elevated the expression level of miR-27a-5p at 4 h in hDPCs (Fig. 1a). Hematoxylin and eosin (H&E) staining showed that the rat pulpitis tissue after experimentally-induced showed a typical inflammatory reaction, with blood vessel dilation and inflammatory cells infiltration (Fig. 1b). The in vivo testing showed that miR-27a-5p expression levels increased significantly after 6 hours of LPS treatment (Fig. 1c). In addition, the mRNA expression levels of IL-6, IL-8, and MCP1 in hDPCs were all significantly increased in response to LPS stimulation (Fig. 1d). LPS significantly promoted NF-κB activity in hDPCs (Fig. 1e), and this was effectively blocked by BAY 11-7085 (Fig. 1e). The application of BAY 11-7085 significantly downregulated LPS-induced IL-6, IL-8, and MCP1 expression (Fig. 1f) as well as LPS-induced miR-27a-5p expression in hDPCs (Fig. 1g).
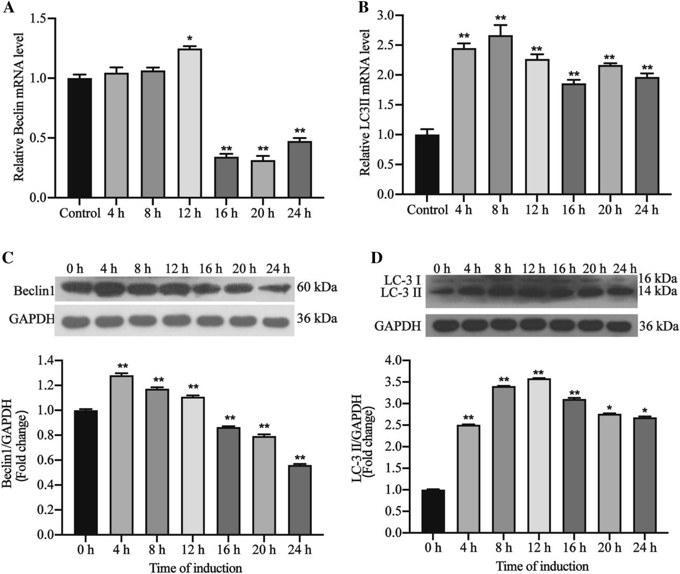
Autophagy Related Factors Induced by LPS in hDPCs
Lipopolysaccharides (LPS) from Gram-negative bacteria induce inflammation, including pulpitis. Autophagy in human dental pulp cells (hDPCs) promotes cell survival under stress. Huang et al. explored whether LPS induces autophagy in hDPCs and whether mitogen-activated protein kinases and NF-κB signaling are involved.
First, to determine if LPS treatment can induce autophagy in hDPCs, the expression levels of beclin1 and LC3II at different time points (4, 8, 12, 16, 20, 24 h) were examined using Western blotting and PCR. The mRNA and protein expression levels of Beclin1 and LC3II were found to be increased after stimulation with LPS (Fig. 2A, B). The expression of Beclin1 protein reached its peak at 4 h, while the expression of LC3II protein reached its peak at 12 h (Fig. 2C, D). The mRNA and protein expression levels of Beclin1 were significantly increased from 12 h and 4 h, respectively, and then decreased. The mRNA and protein expression levels of LC3II were significantly increased from 4 h and were maintained at high levels, and the protein expression levels were significantly increased and peaked at 12 h.
Ask a Question
Write your own review

