
Human Skin Cells (Fibroblasts,Postnatal)
Cat.No.: CSC-7856W
Species: Human
Source: Dermis; Skin
Cell Type: Fibroblast
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
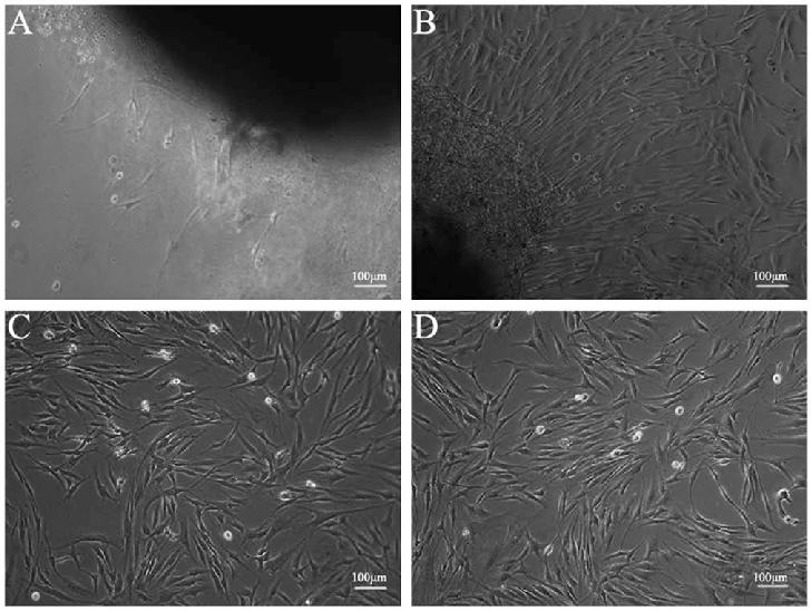
Development period: Postnatal
Human Postnatal Skin Fibroblasts human skin fibroblasts obtained from postnatal human skin (usually neonatal foreskin) by enzymatic dissociation (dispase or collagenase digestion) into dermal fibroblast and epidermal/ECM components. This method yields cells with preserved physiological characteristics, distinct from adult counterparts due to longer replicative lifespan.
Postnatal dermal fibroblasts function to create and remodel the extracellular matrix, and in the context of normal skin, express collagen, elastin and fibronectin, and play key roles in wound healing, tissue regeneration, skin homeostasis through paracrine secretion and through interactions with the ECM. As a result, these cells have been used broadly in the biomedical field for modeling the human skin, and have particular use in studying skin aging and regeneration, modeling and treating skin fibrosis, and in basic skin biology research. These cells have also been used in toxicity screening assays, disease modeling, and the development of tissue-engineered skin replacements, and personalized cell-based therapies.
Effect of the Most Common Wound Antiseptics on Human Skin Fibroblasts
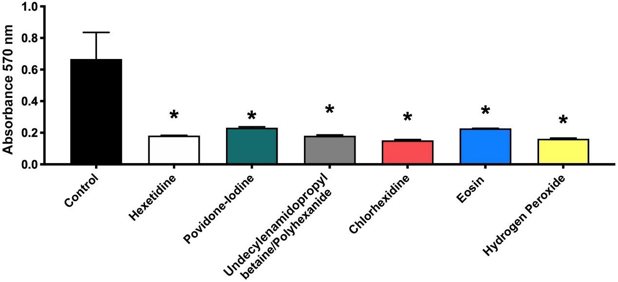
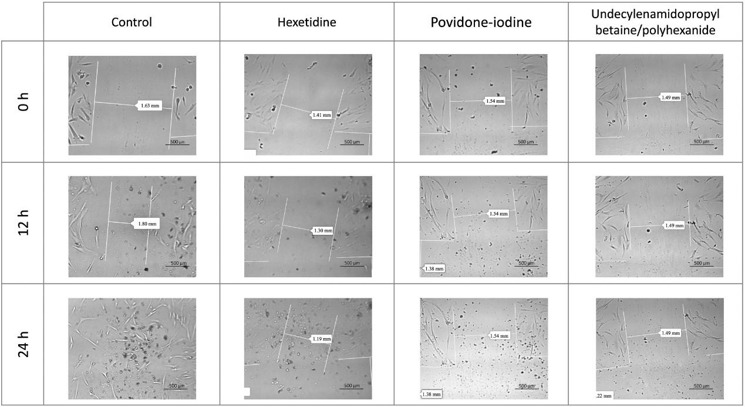
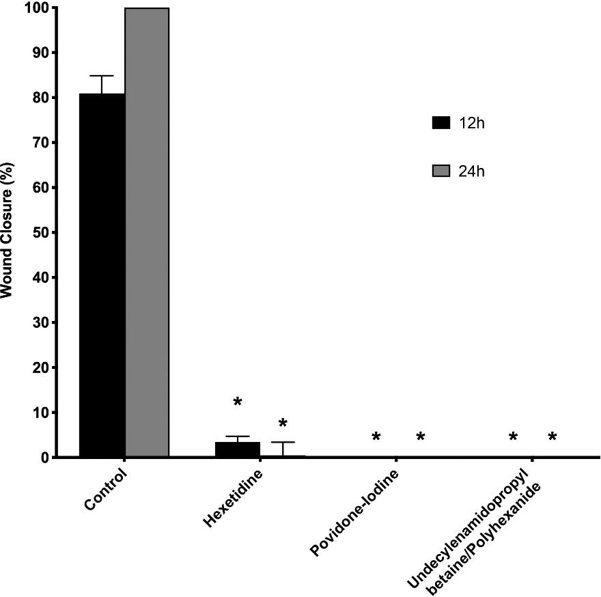
Antiseptics are used for the cleansing of acute or chronic wounds to eliminate micro-organisms from the wound bed. However, they have effects on the skin cells. To determine the effects of hexetidine, povidone-iodine (PI), undecylenamidopropyl-betaine/polyhexanide (UBP), chlorhexidine, disodium eosin and hydrogen peroxide on human skin fibroblasts.
Treatment for 1 min with each antiseptic (hexetidine, PI, UBP, chlorhexidine, disodium eosin or hydrogen peroxide) exerted a significant inhibitory effect on fibroblast viability compared with untreated controls (Fig. 1). The in vitro wound healing assay results (Figs 2 and 3) showed a significant reduction in percentage wound closure compared with controls at 12 h and 24 h after treatment with hexetidine. Cells treated with PI or UBP showed no migration capacity at 12 or 24 h post-treatment, and also exhibited significantly reduced percentage wound closure compared with controls. This assay could not be conducted in fibroblasts treated with chlorhexidine, hydrogen peroxide or disodium eosin due to the cytotoxicity of the treatment. The above results indicate that all antiseptics significantly reduced the viability of human skin fibroblasts compared with controls.
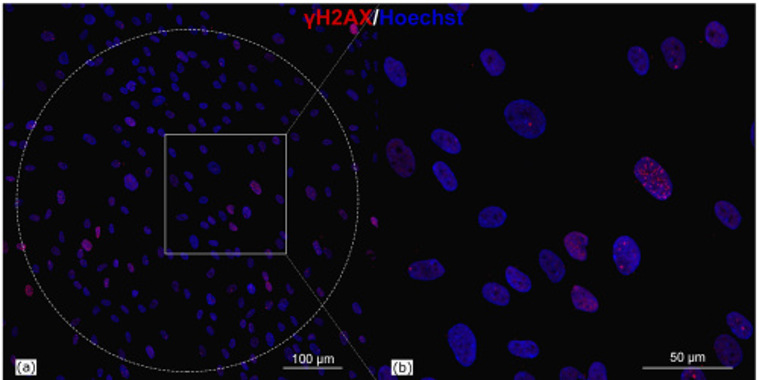
Formation of Histone Н2АХ Phosphorylation Foci (γH2AX) in Human Skin Fibroblasts
Terahertz (THz) radiation, a non-ionizing radiation (NIR) between 0.3 and 10 THz, has broadened its applications in spectroscopy and microscopy. However, the safety of high-intensity THz radiation is still under discussion, with evidence showing potential cell damage and DNA alterations. Sitnikov et al. investigated the molecular-cellular mechanisms of human skin fibroblasts' reaction to high-intensity pulsed THz radiation.
As previously noted, measuring histone H2AX phosphorylation on serine 139 is a highly sensitive indicator of genotoxicity. In this study, they assessed the number of foci formed in human skin fibroblasts treated with high-intensity THz radiation of various parameters. The immunocytochemical staining results are shown in Fig. 4, with the dotted circle indicating the THz-exposed area. The number of foci varied among cells, likely due to both natural processes (cell cycle state, cellular senescence) and the effect of THz radiation. To account for this, they calculated the relative number of foci per irradiated cell. To minimize variability from different donors, they used cells from the 3rd to 5th passage of the same donor in all experiments.
Ask a Question
Write your own review
