
Mouse Cervical Epithelial Cells
Cat.No.: CSC-C9383W
Species: Mouse
Source: Cervix; Uterus
Morphology: Cobble-stone like
Cell Type: Epithelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Mouse cervical epithelial cells are epithelial cells derived from the cervical part of the reproductive system. The cervix is an organ that connects the uterus and vagina. The epithelial cells line up the inner surface of the cervix continuously to form a continuous sheet in both the endocervical and ectocervical regions. Under microscopic observation mouse cervical epithelial cells appear tightly arranged in multiple layers forming a continuous sheet. The tight cell-to-cell arrangement prevents pathogen infection into the uterus. In addition to this, cervical epithelial cells also participate in the local immune response by secreting cytokines and chemokines that modulate immune cell activity. They also secrete mucin with different properties at various stages of the menstrual cycle which aids in the transport of spermatozoa and repair of the endometrium.
Cervical cancer is one of the most prevalent cancers in women. Mouse cervical epithelial cells are often used for setting up animal models to study tumorigenesis, progression, and treatment. The epithelial cells of the cervix are involved in several physiological and pathological events of the reproductive system, thus are also studied for pregnancy, parturition, and miscarriage events.
Analysis of the Accumulation and Neutral Lipid Content of LDs in Epithelial Cells
Although earlier studies showed that progesterone (P4) could induce production of prostaglandin (PG) E2, the mechanism by which P4 mediated PGE2 synthesis has remained unknown. In the present study, Zhang et al. set out to further characterize the relationship among P4, LD and PGE2, with the goal of shedding new light on the mechanism of PGE2 synthesis in reproductive epithelial cells. Cervical epithelial cells obtained from mice during the follicular phase were cultured in vitro and then treated with different concentrations of P4 (5, 10 and 20 nM). The result of fluorescent microscopy (Fig. 1a) and the histogram of the flow cytometry result (Fig. 1d) showed that the total quantity (Fig. 1b, c) of LDs labelled with BODIPY 493/503 was significantly decreased in primary murine cervical epithelial cells after treatment with 5 or 10 nM P4. However, 20 nM P4 had no significant effect on the total quantity of LDs as compared with the control group (0 nM P4).
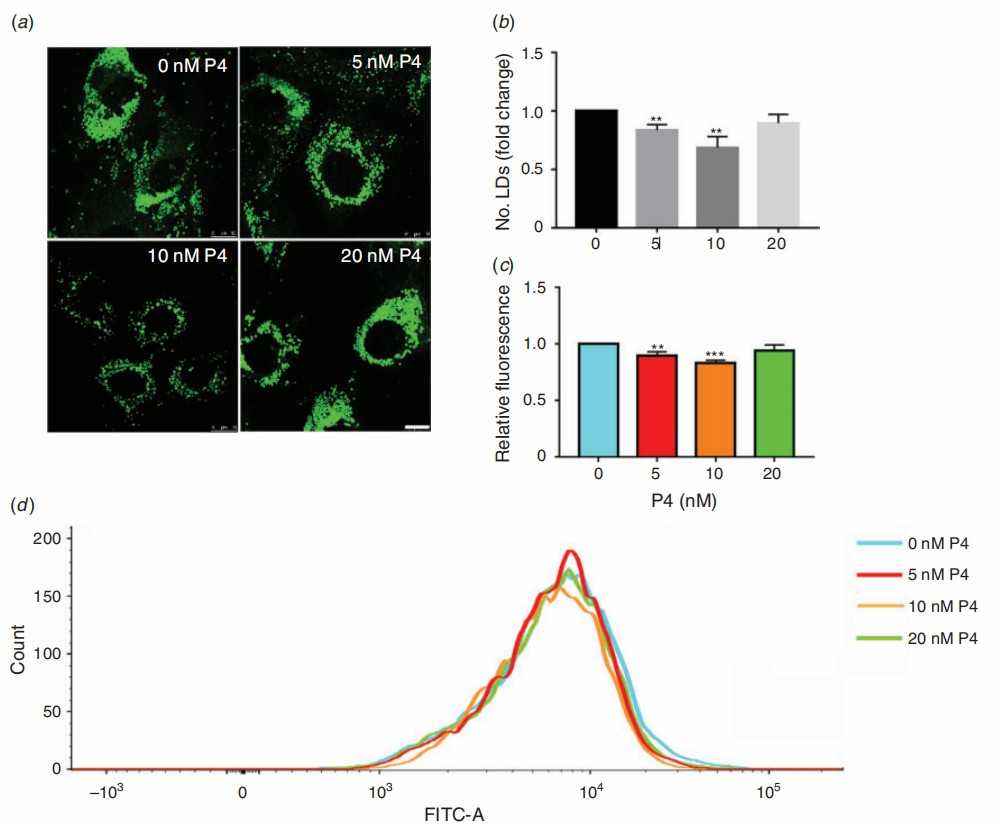 Fig. 1. Quantification and visualisation of intracellular neutral lipid droplets (LDs) in primary mouse cervical epithelial cells treated with different concentrations of progesterone (P4) (Zhang H Y, Su F, et al., 2021).
Fig. 1. Quantification and visualisation of intracellular neutral lipid droplets (LDs) in primary mouse cervical epithelial cells treated with different concentrations of progesterone (P4) (Zhang H Y, Su F, et al., 2021).
Hyperactivation of YAP1 Is Sufficient to Induce Cervical Cancer In Vivo
Most HPV infections don't cause cervical cancer, suggesting genetic susceptibility plays a key role. He's team used transgenic mouse models, including cervical epithelium-specific YAP1 hyperactivation and HPV16 E6/E7/YAP1 double-knockin mice, combined with in vitro/vivo mechanistic studies, investigating YAP1's role in HPV-independent cervical carcinogenesis and its synergy with HPV.
s mentioned previously, they first started to understand the role of YAP1 in cervical carcinogenesis, by generating a mouse model for cervical epithelial cell-specific expression of YAPS127A (Fig. 2A). PCR genotyping confirmed YAPS127A transgene integration (Fig. 2B). At high dose of doxycycline (2.0 mg/mL), the entire body showed multi-organ hyperplasia, and the mice died quickly. This was improved by reducing the doxycycline concentration to 0.05 mg/mL, which eliminated other systemic abnormalities without altering YAPS127A expression levels in the cervical tissue (Fig. 2E). As early as 2 months, cervical epithelial hyperplasia was observed in low-dose Dox-treated KRT14-YAPS127A mice (Fig. 2F). Most mice developed invasive cervical tumors at 6–8 months (Fig. 2C, D, F). The majority of mice developed ureteral obstruction due to cervical cancer expansion, which mimicked a metastatic human cervical cancer (Fig. 2D). After 13 months, 50% of the mice were dead (Fig. 2G). The tumors showed high expression of the cervical cancer-associated biomarkers Ki67, P16INK4A, ΔNp63, EGFR, Pan-KRT by IHC. In contrast to TP53 inactivation in human cervical cancer, TP53 expression level was not altered in these tumors. Taken together, these data demonstrated that KRT14-YAPS127A mice develop CVSCC.
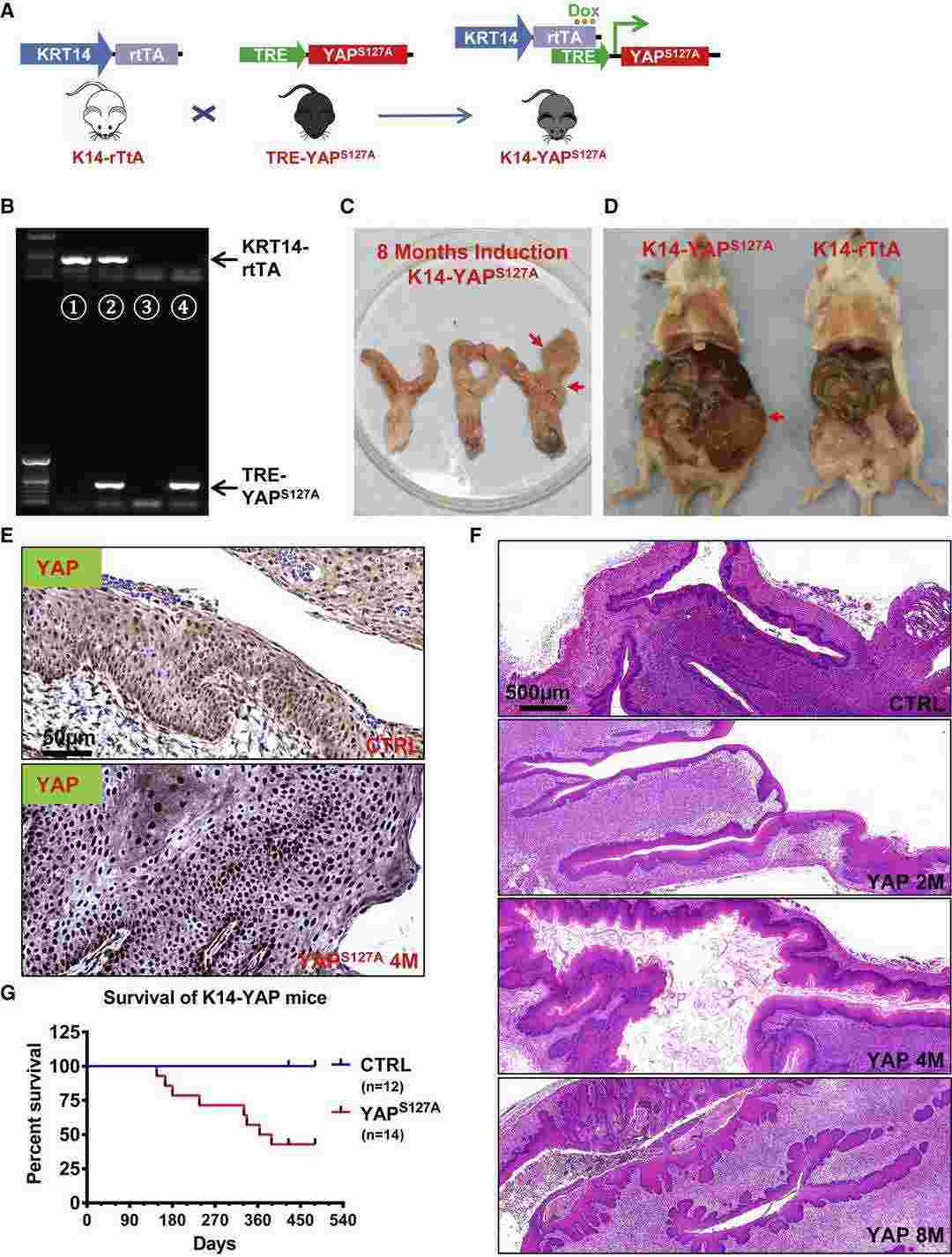 Fig. 2. Hyperactivation of YAP1 Induces Invasive Cervical Cancer in Mice (He C B, Lv X M, et al., 2019).
Fig. 2. Hyperactivation of YAP1 Induces Invasive Cervical Cancer in Mice (He C B, Lv X M, et al., 2019).
Ask a Question
Write your own review


