
C57BL/6 Mouse Primary Colonic Epithelial Cells
Cat.No.: CSC-C4273X
Species: Mouse
Source: Colon; Intestine
Cell Type: Epithelial Cell
- Specification
- Background
- Scientific Data
- Q & A
- Customer Review
Mouse Primary Colonic Epithelial Cells can be used in assays of cell to cell adhesion and migration. Standard biochemical procedures performed with epithelial cell cultures include RT-PCR, Western blotting, immunoprecipitation, immunofluorescent staining or immunofluorescent flow cytometry or generating cell derivatives for desired research applications.
The primary colonic epithelial cells from C57BL/6 mice are extracted from the tissue of their colon. The innermost colon layer contains columnar epithelial cells that function to absorb water and electrolytes. These cells maintain regular morphology and display elongated columnar shapes with smooth surfaces that help them form tightly packed cell layers. Colonic epithelial cells safeguard intestinal barrier integrity as they absorb water and electrolytes and participate in immune response functions. These cells might help control the balance of microbes in the intestinal tract.
Researches employ these cells to investigate disease processes including colitis and colorectal cancer. For instance, mouse models treated with oral Akkermansia muciniphila or AOM/DSS show significant cellular proliferation which serves as an experimental platform to examine gut microbiota disease relationships. C57BL/6 mice serve as a standard genetic background so researchers often use these cell lines to study how gene knockouts or knock-ins affect colonic epithelial function.
TRPV4-mediated increase in cytosolic Ca2+ ([Ca2+]i) and/or current responses in mouse primary colonic epithelial cells and CCD 841 cells
Purinergic signaling, involving ATP release, is crucial in gastrointestinal functions, affecting nerve signaling and peristalsis. ATP is stored in vesicles via the ATP transporter VNUT, and its release can be modulated by TRPV4 channels, which are activated by mechanical and chemical stimuli. TRPV4 and VNUT are known to mediate ATP release in various epithelial cells. Mihara et al. aims to determine if clodronate, a VNUT inhibitor, can block ATP release induced by TRPV4 activation in human gastrointestinal cells, thus presenting a potential therapeutic avenue for treating visceral pain.
Previously, they confirmed TRPV4 expression in mouse and rat gastric epithelial cells. To verify TRPV4 in primary colonic epithelial cells and CCD 841, a human colonic cell line, they used a fluorescent Ca2+ -imaging system with TRPV4 agonists GSK101 and 8,9-EET. [Ca2+]i responses in WT colonic cells were significantly increased with GSK101 (30 nM) compared to TRPV4-KO cells (p<0.05) (Fig. 1A), showing TRPV4 expression. Human CCD 841 cells required 300 nM GSK101 to increase [Ca2+]i, indicating lower expression (Fig. 1B). Clodronate-liposomes didn't inhibit TRPV4 activity. We determined GSK101's EC50 (231.3 nM) and inhibitor RN1734's IC50 (702.6 pM) (Figs. 1C and D). TRPV4 responded to 8,9-EET with an EC50 of 111.1 nM (Fig. 1E), and was inhibited by RN1734 (Fig. 1F), confirming TRPV4's role.
![TRPV4 facilitates an elevation of cytosolic Ca2+ concentration ([Ca2+]i) in both mouse primary colonic epithelial cells and CCD 841 cells.](/upload/image/26-c57bl6-mouse-primary-colonic-epithelial-cells-1.jpg) Fig. 1. TRPV4-mediated increase in cytosolic Ca2+ ([Ca2+]i) in mouse primary colonic epithelial cells and CCD 841 cells (Mihara H, Uchida K, et al., 2018).
Fig. 1. TRPV4-mediated increase in cytosolic Ca2+ ([Ca2+]i) in mouse primary colonic epithelial cells and CCD 841 cells (Mihara H, Uchida K, et al., 2018).
DPCA Repairs the Colon Lining through Activation of Epithelial Cells
IBD is marked by recurrent inflammation and ulceration, severely impacting patients' lives. Current treatments manage symptoms but often fail to heal the intestinal mucosa fully, necessitating novel therapies to facilitate tissue regeneration. DeFrates et al. aimed to assess the efficacy of a new prolyl hydroxylase inhibitor, DPCA, delivered through a PEG-DPCA hydrogel, to enhance tissue regeneration and repair colon damage in experimental colitis models.
Previously, DPCA was shown to promote a similar effect in a murine ear hole wound, where re-epithelialization is seen just two days after injury. To better understand the mechanism driving this effect, they treated primary colonic epithelial cells from mouse colons with DPCA, observing a morphological shift from cuboidal to spindle-like, indicative of epithelial-mesenchymal transition (EMT) (Fig. 2A). This change aligns with heightened HIF-1α signaling. DPCA-treated cells exhibited increased vimentin expression, actin depolymerization, and decreased epithelial markers like E-cadherin (Fig. 2B and C). Vimentin was robustly expressed in treated colitic mice around healing lesions, contrasting with reduced expression in untreated controls (Fig. 2D). This supports that HIF-1α may drive EMT through transcription factors like Slug and Twist1 (Fig. 2B), despite no significant increase in SNAI1 or TGFB.
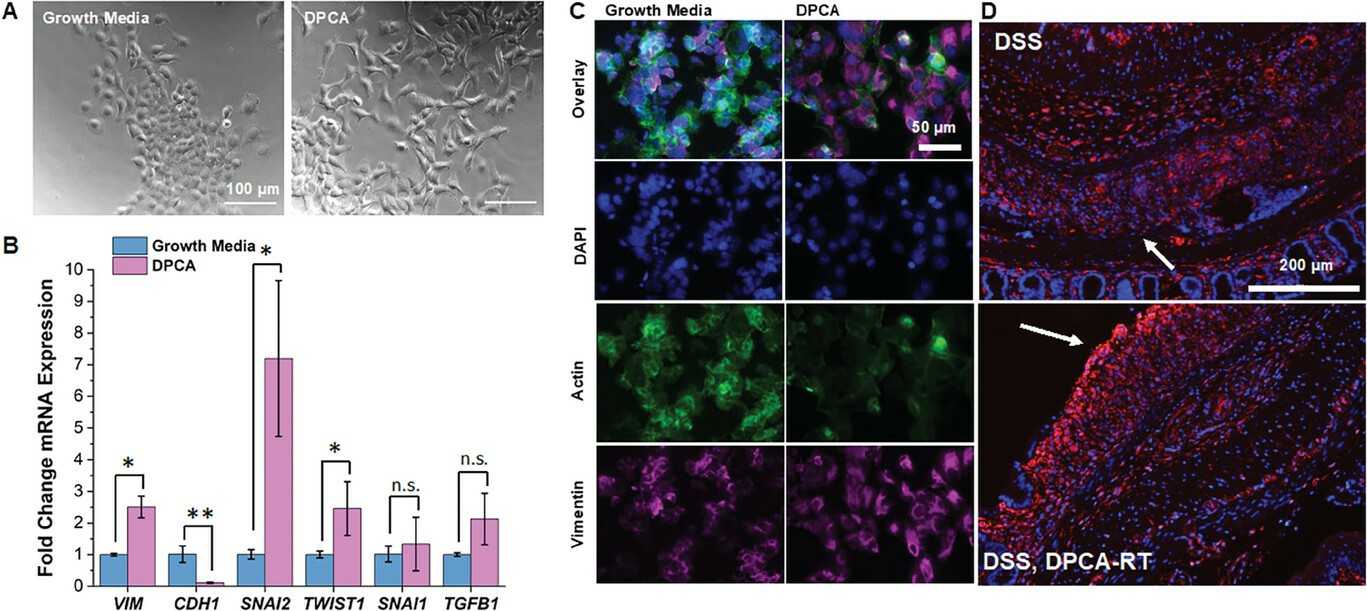 Fig. 2. DPCA repairs the colon lining through activation of epithelial cells (DeFrates K G, Tong E, et al., 2024).
Fig. 2. DPCA repairs the colon lining through activation of epithelial cells (DeFrates K G, Tong E, et al., 2024).
Ask a Question
Write your own review




